The first slide in the Eye & Ear Foundation’s June 13th webinar, “Salivary Gland-Sparing Surgery and the Role of Sialendoscopy,” featured the cylinder scope. “This long instrument is the most novel new technology that’s come out in the last couple of years,” said Shaum Sridharan, MD, Associate Professor in the Department of Otolaryngology-Head and Neck Surgery and the Associate Director of the Advanced Head and Neck Surgical Oncology Fellowship.

This scope is a telescope that is fed into the salivary gland and has multiple channels. Though the images are small, surgeons are able to see within the salivary gland and use interventions like balloon dilation to remove stones. Botox can also be used to turn off the salivary gland and reduce the sequela of some of the chronic inflammatory diseases that are seen.
This scope is used in gland-sparing surgery, which involves the ability for surgeons to intervene on the salivary glands without destroying their function. “Basically, we’re able to use minimally invasive techniques and novel treatment strategies in order to help maintain the function of the gland while still being able to remove tumors or stones or change the function of the gland after sequela from other treatment,” Dr. Sridharan said.
Treatment Dilemma
Dr. Sridharan shared a case of a 56-year-old man with a history of hypertension and GERD. He also had persistent right sided neck swelling and pain with meals. This is very uncomfortable and not easy aesthetically. He was told by two other ENTs that he needed his submandibular gland excised and was sent to Dr. Sridharan for a second opinion. Later in the talk, Dr. Sridharan shared what happened with this case – stay tuned.
Salivary Glands
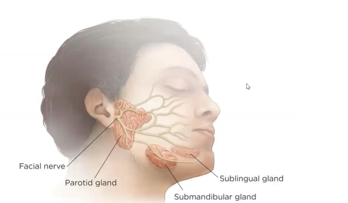
Salivary glands include the facial nerve, parotid gland (on the side of the cheek right in front of the ear), sublingual gland (the smallest), and the submandibular gland. There are also minor salivary glands that are extremely small and present throughout the mouth.
The facial nerve supplies the innovation to muscles across the face to get the face to actually make movement like smile, raise your eyebrows, and close your eyes. “This is just to illustrate that the glands are in the sort of this danger zone where you have these nerves that are coming across it and must be dealt with when you want to manage pathology within these glands,” Dr. Sridharan said.
Parotid Anatomy & History
Nicolaus Stenonius (1660), studied anatomy under Gerard Blasius, with a focus on the lymphatic system. He discovered the “ductus stenonianus” in sheep, dog, and rabbit heads. He actually was dissecting sheep and saw there was an opening that no one had described or understood. He started probing this duct and opening, and found it actually connected to the salivary gland.
This duct is called the stencils and is about three inches in width. It crosses over this big muscle pier and enters into the submandibular gland, the second biggest of the major salivary glands.
Submandibular Gland Anatomy & History
- Described by Thomas Wharton in 1659
- 5 cm long, 4mm wide
- Cross by the lingual nerve
Sublingual Ductal System
Bartholin’s duct is what connects it to the oral cavity. This one is not able to be navigated much like the other two.
Differential Diagnosis
“We are thinking about a lot of different things,” Dr. Sridharan said. “Not everybody that has salivary gland swelling is really having stones or something obvious, so we have to be thorough doctors and really think about what it could be.”
Here is a list of differential diagnoses for surgeons to consider:
- Infectious (acute) cause – Bacterial or viral disease
- Inflammatory cause – Sialolithiasis, radiation-induced disease
- Autoimmune cause – Sjogren disease, lupus
- Granulomatous cause – Tuberculosis, tularemia, sarcoidosis, catscratch disease, actinomycosis
- Drug-related cause – Thiourea
- Neoplastic (benign) cause – Pleomorphic/monomorphic adenoma, oncocytoma, ductal papilloma, hemangioma, foreign body, ranula, lymphoepithelial cyst
- Neoplastic (malignant) cause – Adenoid cystic carcinoma, mucoepidermoid carcinoma, adenocarcinoma, undifferentiated carcinoma, malignant oncocytoma, squamous cell carcinoma
- Endocrine cause – Hypothyroidism, diabetes mellitus
- Metabolic cause – vitamin deficiency, cirrhosis, obesity, bulimia, malabsorption
Sialoithiasis
The most common reason Dr. Sridharan gets referred patients is salivary stones. The medical term for this is sialoithiasis. They can obstruct the outflow of the salivary gland. Size and location matter. These stones are usually kind of yellow in color. They can obstruct the salary flow, but sometimes they are too small to obstruct the flow or they are in a position where they can jostle around and cause intermittent symptoms.
If the stones are very far, closer to the mouth, inside of the gland, there are different types of approaches.
Epidemiology
- 1 in 15 – 30,000 incidence of stones
- Autopsy studies of sialolithiasis show presence in about 1% but location and symptoms not addressed
“That’s not very common, but we tend to see a lot of it here at the University of Pittsburgh because there’s nobody else taking care of these patients [nearby],” Dr. Sridharan said.
A mineral composition of salivary gland x-ray diffraction and chemical analysis of stones found that there are 32 submandibular stones, with hydroxyapatite most frequent with magnesium-substituted whitlockite co-phase. There are six parotid stones, apatite, magnesium substituted whitlockite and octacalcium phosphate major crystalline phases. Brushite was rarely found, and whitlockite was mostly in the central regions of the stones not in the outer crusts.
While these are made up of different substances, they are firm and hard. You can crush them when you take them out of the body or with a laser. You can usually avoid them, but they are pretty firm and cause symptoms.
Radiology for Salivary Glands
Usually, these gland pathologies are diagnosed with history and imagine. Plain film imaging is difficult to interpret sometimes. Plain films are 20-70% radio-opaque. In CT imaging, not all stones are radio-opaque. Sometimes the dots can be even smaller than detected on the CT scan. A lot of it sometimes is based on the clinical picture and the obstruction and some history of whether they’ve had stones before.
Another way to image patients is via sialogram, which is invasive, and cannot be done during acute infection. It is challenging to perform and read, as contrast has to be injected into the duct and back through the salivary piping into the gland.
MRI sialography involves more interesting but less commonly used technologies. It is non-invasive. It is probably done less often because most of the time people use the endoscope to assess the gland, and the CT scan is quite good. In a pinch or when things are not really making sense, this is very good, and can be done at Pitt usually in coordination with the radiology department. It uses the natural texture of saliva to identify how the salivary flow is being inhibited or where it is pulling and can provide a lot of information.
Marchal and Becker did a survey of 64 glands:
- 23 sialolithiasis
- 9 sialolithiasis and stenosis
- 11 stenosis only
- 2 early sjorgrens syndrome
- 16 normal
In terms of accuracy:
- Stenosis
- Sensitivity – 100%
- Specificity – 93%
- Positive – 87%
- Negative predictive values – 100%
In-office ultrasound can identify salivary stones and masses and can be performed on the same day as an office visit. This is easy and great as an adjunct for when stones are being taken out so that there is a visual representation of the stone from both directions. Patients love it because they get instant feedback. It can pick up masses and signs that there is chronic inflammatory disease. “It is underutilized in the U.S.,” Dr. Sridharan said. “We try to use it on all our salivary gland patients here in the clinic.”
What Imaging to Use
- CT best assessment of inflammatory diseases
- MR best for salivary gland tumors
- MR sialography will replace sialography
- Ultrasonography underused in US, in experienced hands may supplant CT/MR
Sialendoscopy
Over the course of about two decades, sialendoscopy has advanced from a very primitive mechanism to what exists now.
A timeline:
- 1991 P Katz radiologist using nude fiber no rinsing mechanism
- 1992 Iro shock wave lithotripsy
- 1993 Koningsberger combined flexible scope and lithotripsy
- 1996 Marchal developed set Karl Storz
- NEMJ on State of the Art (1999)
- 2004 Zenk and colleagues slightly flexible semi rigid endoscope with high-quality imagine (6,000 pixels)
- 2006 Nahlieli rigid mini endoscope to treat salivary disorders
- 13 year experience with >80% success in treating obstructive pathology
- Iro, Zenk, Escudier, Nahlieli, Capaccio, Katz, Brown, McGurk “Outcomes on Minimally Invasive Management of Salivary Calculi in 4,691 Patients” Laryngoscope 119: 263-8, 2009
Dr. Barry Schaitkin was one of the early adopters.
Sialendoscopy can be performed in the OR or in the clinic. Other features include:
- MAC vs general anesthesia
- Utilize working channel and irrigation channel – nice because you can feed larger instruments through the working channel to get stones and other things out of the patient’s body
- Varying sizes of scopes (all fragile!)
The process has to be done with care. It can be five minutes or can take a lot longer. Most of the instruments on set are valuable and can be used in conjunction:
- Dilators/bougies
- Endoscopes
- Wire basket
- Forceps/grasper
- Balloon dilator
“Newer instruments are being developed all the time,” said Dr. Sridharan. “We’re trying to use what’s the latest and try to help our patients and maintain this minimally invasive [procedure]. The way we think about or the way I teach the residents is the size of and the location of the stone really really matters.”
Small Stones
- < 4 mm width (can be elongated)
- Can require sialodochoplasty
- Positioning and stabilizing stone
You can put the endoscope in, feed a wire through, and pull the stone out. It is minimally invasive because you do not have to do much – no cuts in the mouth or on the actual opening. In some cases, you can actually grab the stone and better position it.
Large Stones
- Often benefits from combined approach utilizing sialendoscopy and open surgery
- Can still maintain function of the gland
- Consider stenting when appropriate
For medium sized stones, you can repeat the same procedure where you can use the basket and cut down or sometimes you can palpate the stone in the floor of the mouth, make a cut and take it out that way. The endoscope is so valuable because you can actually follow the duct even after you have taken the stone out with an open approach.
If you leave other stones behind, that is when you run into a lot of problems and have to do a revision surgery. The best is to do it right the first time. You can make strategic decisions on the patient in order to remove the stone and get the best of the gland without having a major cosmetic deformity.
Submandibular Technique (Marchal)
- 2 cm incision over the stone/light
- Assistant elevates submandibular gland
- Isolate and retract the lingual nerve
This usually doesn’t cause any difficulty to speaking.
Parotid Stone
- Place scope at the level of stone or stenosis
- Raise a parotid skin flap via face lift incision
- Locate the light
- Raise SMAS flap
- Enter duct after identification of buccal branch facial nerve
“The reason why we don’t make a cut directly over the light is because that’ll cause a scar on the patient’s face,” Dr. Sridharan said. “So we’d rather have this incision that’s much more hidden in order to have the best cosmetic outcome for the patient.”
Duct Identified
- Incise duct
- Remove the stone
- Endoscope rest of duct
- Sometimes externally
- Closure with 7-0 nylon
- Marchal suggests reduction of redundant mucosa if necessary or
- Vein graft patch if duct stenotic
- Scope can irrigate to assess integrity of repair
“We use the endoscope to make sure there are no other stones and then we can actually close the duct using microsurgical techniques with a very tiny needle,” Dr. Sridharan said. “You can either patch it or you can close it completely and sometimes you can even place a stent that stays in there for a couple of weeks to maintain the patency. Then you can do a complicated multi-layer closure to make sure that no saliva leaks out of the wound.”
This is the standard approach for larger, private stones, especially ones that are not very close to the very front by the mouth opening.
If this is complicated, why not just remove the gland? Why not just take out the tissue?
- Incision on the neck
- Risk to facial nerve
- Hematoma/abscess
- Lingual nerve injury
- Hypoglossal nerve injury
There will definitely be a scar. It is not uncommon for the facial nerve to be dissected and removed to get the gland out. Patients can have temporary or permanent facial nerve weakness from the operation.
“You really don’t want to be messing with those nerves unless you really have to,” Dr. Sridharan said.
Sometimes Gland Excision
- Large stone at the Hilum of SMG – remove the stone and gland together
- Persistent symptoms (stenosis, prolonged hx of obstruction)
- If performing parotidectomy for inflammatory disease, often you need to do a total parotidectomy
This is that marginal mandibular weakness, which is hard for patients to have this lift not kick out as much so when they smile, this slip is not moving as much. The patients can bite on their lip. They don’t like some of the cosmetics. Sometimes this is very disturbing to the patients. “It’s something we’d like to avoid if we can by doing these minimally invasive techniques,” said Dr. Sridharan.
When you have a stone that is within the salivary gland, your hand is a little bit forced. You sort of have to remove the gland. It is more common to have facial weakness in this operation. “We like to avoid doing major gland operations unless we really have to,” Dr. Sridharan added.
Non-Stone Sialendoscopy
- Stenosis
- Sjogren’s Disease
- Scar
- Juvenile recurrent parotitis
- Post-radioactive iodine
Some of these patients have significant gland dysfunction, so the sialendoscope is used to really wash out those glands and try to improve salivary function.
Chronic Obstructive Parotitis: Strictures of Stenson’s Duct. Our Sialoendoscopy Experience
- Most salivary gland swellings are non-neoplastic & generally due to obstructive conditions
- Strictures and kinks are a frequent cause of obstructive sialoadenitis
- Unlike sialolithiasis, strictures frequently involve the parotid gland system and mainly affect women
- 10 years ago, the published scientific data had underestimated this condition
Dr. Sridharan sees a lot of patients that have no stones but recurrent swelling. Most times, 9 out of 10, they say they feel so much better having had this procedure.
Adjunct Procedures
- Balloons for dilation
- Stenting
- Most improve with serial dilation and saline infusion (Steroids)
- Around 80% need only 1 procedure
Patients don’t love having stents because it rubs on their tongue a bit. But if they can keep that in for a week or two, it actually makes a big difference. Probably the most valuable thing is just flushing the gland with saline and getting all the debris and gunk out of the gland – patients feel a lot better.
Future Directions
- Patient-reported outcomes – “We need to make sure that we’re really affecting patients’ lives and showing value to what we’re doing,” Dr. Sridharan said.
- Multi-disciplinary care clinic – one-stop shopping type of scenario
- In-office procedures – like to do more of these as our Shadyside space gets built out and there is more procedural space
- Multi-institutional research – trying to study these combined hybrid approaches. “We have about 10 institutions sending us data to see if we can publish on what would be the best practices,” Dr. Sridharan said.
Dr. Sridharan gave the example of a salivary gland quality of life assessment. The test is called the spit or the obstructive salivary problem impact test. Patients take this quick survey of their symptoms and then physicians track how they’re doing. This will be used a lot. This is being used in a couple of institutions and the first paper on the originator for this and the spit questionnaire was also co-authored by Dr. Schaitkin.
In-office Procedure
In office procedures are great. “If we can do a lot of the same things that we could do in the operating room in the right patient in the office saves a lot of time and money,” Dr. Sridharan said. A study done by a group out of UNC showed that the procedure times were so significantly different between the two groups because of the time to go into anesthesia, time to wake up, time of the actual procedure, post procedure time, etc. They amounted to be 40 min vs 276 min for the patient. The surgical time is not hugely different. It is different than the operating room. “I think we really should be taking into account in the right patient who can tolerate in the office procedure,” Dr. Sridharan said. Cost-wise, there is also a stark difference of $1,000 vs $150.
Conclusions
- Sialendoscopy is effective and has developed over 25 years
- Can be used as a primary modality or part of combined approach
- Can improve quality of life in patients with chronic disease
Dr. Sridharan then returned to the case he mentioned in the beginning. The man’s stones were removed with the cylinder scope. Then more came into view and came out in rapid sequence – at least 20 stones were removed. The patient is still doing well and enjoying eating without having a constantly swollen gland. He also does not have the scar or facial weakness.
“We’re thankful for this technology,” said Dr. Sridharan. “We are trying to push the envelope here at the University of Pittsburgh.”