Advancements in glaucoma treatment and research was the topic of the Eye & Ear Foundation’s November 15th webinar.
Ian Conner, MD, PhD, is Assistant Professor of Ophthalmology, Director of the Glaucoma Service, and Fellowship Director at the University of Pittsburgh School of Medicine. He also serves as a Diplomate on the American Board of Ophthalmology. “I really believe in this mission and idea of interventional glaucoma care,” he said. “Glaucoma traditionally has been treated as a medical disease and then only when it gets pretty bad do we consider surgery. But there is a paradigm shift occurring right now in the field of glaucoma. We’re starting to think of more than surgical disease. It is a really exciting time for us and hopeful time for patients. We expect that we may even be able to begin to turn the tide and regain some vision in people who have glaucoma instead of just stopping the damage from getting worse.”
MIGS
Dr. Conner shared how far surgeries have come in the last 10 years or so. There used to be just one choice that involved making a hole in the eye and creating a bypass outflow system to lower pressure in the eye. Now there are a number of less invasive alternatives that have faster visual recovery. They are less powerful than traditional surgery, but they are still a much better, safer, more tolerated option. They fall under the umbrella of microinvasive glaucoma surgery, or MIGS. An important goal is to minimize medication use.
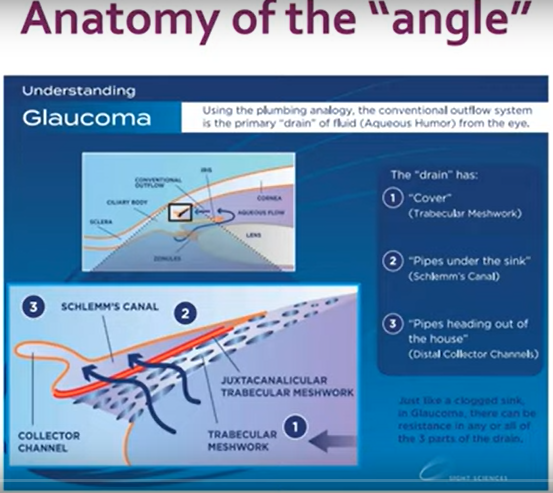
There are many different MIGS options. They deal with the fundamental problem of lowering the pressure in the eye. MIGS has many different targets, with different categories of procedures.
Tailoring Treatment
When examining and thinking about a patient’s specific disease, the surgeon thinks about the different MIGS categories and tries to tailor the treatment accordingly. The most important question is whether MIGS is appropriate for the patient. What is their stage of disease, intraocular pressure (IOP) target, anatomy and type of glaucoma, and reason for surgery? “Just because we can do it doesn’t necessarily mean that we should or must,” Dr. Conner said.
Another question is, “Is the surgery I am doing likely to achieve the outcome that I desire?” Patients with advanced damage, for example, who need IOP in single digits, would not be great candidates for MIGS, just like patients with neovascular glaucoma.
Better MIGS candidates are those with mild-moderate stage disease, whether medically controlled or uncontrolled. Patients with advanced stage disease who are medically controlled, and who need to minimize medications, or who are undergoing cataract surgery.
Outcomes
Dr. Conner said there is a mounting series of evidence that most surgeries have the ability to lower the pressure by 20-30% on average, and usually can lower the medication burden by 20-40% as well.
Surgeries
Dr. Conner described the different kinds of surgeries for open angle glaucomas and closed angle glaucomas. In addition to MIGS, he described replacements for traditional glaucoma surgery including the XEN implant. XEN – the size of an eyelash, made of collagen – is a shunt procedure. Another shunt procedure is PreserFlo, but it is not yet FDA-approved. Disclaimer – minor revisions of these newer shunts is relatively common.
Finally, micropulse glaucoma laser is a safe, external procedure that is good for patients who are poor surgical candidates. It appears to work by contracting the sclera and longitudinal ciliary muscle, opening the canal. It may have a role earlier in the disease and is repeatable.
Summary
As Dr. Conner summarized, “We have many MIGS options, but not all patients are candidates.” Treatment requires a highly individualized approach, and it is important to match the pathology to the procedure. Selection criteria may change as technology evolves.
Retinal Ganglion Cell (RGC) Differentiation and Transplantation
The second part of the webinar was presented by Kun-Che Chang, PhD, Assistant Professor, Department of Ophthalmology, University of Pittsburgh. His current research interests focus on retinal ganglion cell development as well as gene and cell replacement therapies for glaucoma and optic neuropathy. He presented his research on glaucoma and RGC, sharing experimental studies like gene therapy for axon regeneration, RGC survival, RGC replacement therapy, donor cell transplantation for RGC loss, human stem cell differentiation, and donor cell integration.
Two challenging areas have promise: Gene therapy and stem cell transplantation. For gene therapy, long distance axon regeneration is needed, along with a cocktail therapy. Safety of AAV injection in humans must be ensured.
Stem cell transplantation promotes RGC differentiation, involves synaptic connection and injury models. Immunosuppression may be required if cross-species, and FDA regulations must be adhered. Unlike currently available treatments, gene therapy and stem cell transplantation have the potential to actually restore lost vision but are likely still a few years way from clinical use. The UPMC Vision Institute is well-positioned to help pioneer these human trials as the science becomes reality.
More information on UPMC Glaucoma Services