In The Eye & Ear Foundation’s December 14th webinar, “Chronic Rhinosinusitis,” Dr. Eric Wang tackled what he said seems like a common thing yet has a lot of variation and interesting aspects to discuss.
“One of the problems with sinusitis is that term means a lot of different things to a lot of different people now,” said the Executive Vice Chair of the Department of Otolaryngology and Professor in the Departments of Otolaryngology, Neurological Surgery and Ophthalmology at the University of Pittsburgh School of Medicine, and Co-Director of the UPMC Center for Cranial Base Surgery and Director of the Division of Rhinology.
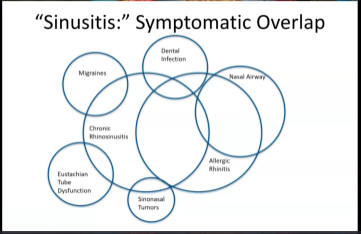
Sinusitis: Symptomatic Overlap
People think a lot of things might contribute to their sinus issues. Dental infection is probably the most common, Dr. Wang said, because the pain hurts in that area. Migraines are also relatively common because the pain that happens is in the four-quadrant distribution that is often attributed to sinusitis. Many times it is, when it is actually a version of a headache.
“The nose is a very simple thing,” Dr. Wang said. It doesn’t have many ways of communicating with us. Whether that’s the ability to breathe because of structure, allergies, inflammation in the nose, or inflammation in the paranasal sinuses, they sometimes all overlap and mimic each other to some degree. Even in rare situations, there are tumors in the nose and paranasal sinuses that mimic sinusitis.
“So, there’s a lot of overlap from a symptom standpoint,” Dr. Wang said. “It’s certainly not any patient’s challenge, but it becomes a diagnostic challenge for us to figure out.”
Chronic Rhinitis and Rhinosinusitis
The four cardinal symptoms of chronic rhinosinusitis are:
- Nasal congestion/obstruction
- Nasal drainage
- Decreased sense of smell
- Facial pressure
Unfortunately, these have a fair amount of Venn diagram overlap. They can either result in chronic rhinosinusitis, sinusitis, or they can just be allergic rhinitis within the nasal cavity itself.
“The symptom overlap is pretty high,” Dr. Wang said. “This is why it’s really hard for our really bright colleagues in primary care medicine to differentiate that.”
First Line Therapy
“Part of the reason we’re able to get away with it a little bit is that the first line therapy for both of these conditions is kind of the same stuff,” Dr. Wang continued. “It’s nasal steroids, like Flonase.” They reduce inflammation in the nasal cavity, and sometimes it also translates to the paranasal sinuses.
Saline – what Dr. Wang calls the teeth brushing of your nose – is a cleansing agent that is also used. He said there is nothing particularly amazing about it. Just getting irritants out of the nose make people feel better.
“The truth is the majority of people in both conditions, whether it’s chronic rhinitis and sinusitis or allergic rhinitis, get better with just these two straightforward nasal medications,” Dr. Wang said. “That’s great. Now I would be out of a job if that was the whole thing.”
Sinus vs Nasal Cavity
Past the first line therapy, the challenge is trying to decipher whether the problem is located within the nasal cavity or in the paranasal sinuses, which are outside the nasal cavity and drain into the nasal cavity. Or is it both? Differentiating this helps healthcare providers consider what second or third line interventions to use. It is not easy as the symptoms are so similar.
What is Chronic Rhinosinusitis? (CRS)
This is when symptoms last for 12 weeks or longer. The symptoms are the four cardinal symptoms mentioned earlier. Drainage can be from the front or isolated to the back. Symptoms do not include headache or facial pain. A CT scan and nasal endoscopy are objective tools used in diagnosis.
Sometimes CRS is not the only diagnosis; it can mean different things. Take primary vs. secondary – is it something that primarily arises from the sinusitis or is it something that can be more global or adjacent? Secondary kinds of CRS can be local pathologies, like the teeth. Secondary CRS has its own characteristics – it is more global, affects the whole body, and the nose is just one area in which the symptoms can manifest. Primary CRS is where the disease process is primarily within the paranasal sinuses and has spread to the nasal cavity.
Basically, the term CRS is not a catch-all diagnosis, but there are subtypes within it that are important to differentiate because the treatments are different.
Secondary CRS: Odontogenic Sinusitis
This is one of the most common forms of secondary CRS nowadays. It essentially means something that arises from the tooth, usually the upper teeth in the upper jaw. It does not tend to manifest with typical dental issues. As the infection pushes against the bone, it ruptures into the sinus, which is a big space. You do not get the typical dental pain issues that are seen in the lower jaw. This can last a long time.
Its most common symptom is extremely thick, bad smelling drainage. This is because teeth have anaerobes or bacteria that survive well without oxygen, which is common in the mouth but not in the nose. Frequently it is only on one side, but sometimes happens in both.
Facial pressure is another symptom. There are other kinds of odontogenic sinusitis besides the infection itself, like dental cysts/tumors, which can grow into the sinuses, or dental implants and sinus lifts.
Treatment is sinus surgery followed by oral antibiotics. The tooth problem still has to be taken care of after, so dental interventions are needed.
Secondary CRS: Fungal Ball
While a fungal ball can start from the teeth, it has characteristic calcifications on the CT scan. Symptoms are similar to odontogenic sinusitis: purulent drainage, facial pressure, and unilateral nasal congestion. This is not a fungal infection – it fills the airspace of the sinuses, starts to erode the bone and push it out.
Sphenoid Fungal Ball
A lot of times, people live with fungal balls for years. They can happen predominantly in the maxillary sinuses, but also back in the sphenoid sinus. This kind of fungal ball results in headaches at the top of the head or the back of the head, along with postnasal drainage. The process is the same – fungal debris that fills up the sinus, acts like a cork, and blocks it off.
Treatment is sinus surgery to remove the fungal ball using tiny telescopes through the nasal cavity. Recovery takes about a month. No antifungal drugs are needed.
“[This kind of surgery] is very rewarding to help people because you make a huge difference in their quality of life,” Dr. Wang said.
Secondary CRS: Cystic Fibrosis and Primary Ciliary Dyskinesia
Cystic fibrosis is a genetic abnormality within the lining where people are not able to push out chloride within the cell membrane. This causes a lot of thickening of secretions that are normally made.
In the nose, we have little hair cells called cilia on top of the nasal lining. They help push mucus towards the back of the throat. It is estimated that we make about 1-2 liters of mucus a day. The idea is that this mucus catches all of the things in the air and captures them, so they don’t get in our lungs. Then the cilia push mucus back to our throat, we swallow it, and it does not hurt us. With primary ciliary dyskinesia, that process does not work. In other words, the cilia do not work. They are there but do not move anything, so all the mucus gets stagnant.
The end result is inflammation and what appears to be an infection in the nose. Unfortunately, there is no cure for primary ciliary dyskinesia. People with it also have problems with pneumonia. Treatment is non-anatomical sinus surgery.
Cystic fibrosis used to limit people’s lives to their teenage years. As treating the infections improved, people were able to live to their 20s and 30s. With lung and pancreas transplants, that extended to the 40s and 50s. The Cystic Fibrosis Foundation was able to come up with a drug that helps the chloride process open so more of it gets into the periphery and the mucus is thinned. Through donations to the CF Foundation, two other things were found to work on this particular protein at the cell surface. Now there is a medication, Trikafta, that has all three of these versions.
“We basically to some degree have controlled cystic fibrosis,” Dr. Wang said. “I used to operate on 20-30 people a year for this condition. Now I think I do one operation a year for it.”
The drug can be taken as young as two years old. As a rhinologist, Dr. Wang said this used to be a real challenge. Now this amazing medication makes a gigantic difference in the lives of 75-80% of patients.
Secondary CRS: Others
Other kinds of secondary CRS could be autoimmune, in which the body fights itself, particularly the vessels within the nose. Two examples of this are granulomatosis with polyangiitis (GPA), formerly known as Wegener’s granulomatosis, and sarcoidosis.
Another kind is when there is primary immunodeficiency, when the body is not able to fight infections.
Primary Chronic Rhinosinusitis
When sinus inflammation primarily arises from the sinuses themselves, that falls in this category. One variant of primary CRS is nasal polyps. Symptoms include nasal congestion, increased rhinorrhea, and decreased olfaction. There is a 0.4-2% prevalence in North America/the United States. Recurrence of polyps are common, driven by Type 2 inflammation. This pattern of inflammation is seen in asthma and atopic dermatitis, which some people have hypothesized that it is a spectrum of diseases.
Nasal Cycle and Normal Sinus Inflammation
Dr. Wang uses the analogy of a scale or seesaw to explain how the nasal cycle works. In an ideal world, he explained, our nose actually needs inflammation because that is the way we clean our nose. We produce mucus that way, which captures the bad things in the air, pushes them to our stomach for us to expel. We need this process where sometimes our nose gets inflamed, cytokines go up, and inflammation occurs. We clear the other things out, which helps us fight infections.
We then have regulatory cytokines that rise and inflammatory cytokines that go down. Now we can breathe better and smell. There is always an up and down balance between the two; one goes up, the other goes down.
In CRS, that process gets broken. Typically, it happens in two peaks. The early 20s is the first one and is smaller. The more common one sometimes happens in the mid-40s-mid-50s. It is not known what breaks the scale. But the inflammatory cytokines go way up, and the regulatory ones go down. The inflammatory process now begins to be dysregulated. This imbalance makes us feel like we have an infection. But it really is not a primary infectious process. We just associate this inflammation with infection.
What is really occurring is a dysregulation of the balance system of necessary inflammation in the sinuses. When that balance gets thrown off, chronic inflammation occurs. In one of its end stages, the pockets of lining or mucosa pooch out and become polyps.
One of the biggest concepts that has advanced since the 80s is that CRS is not an infection that does not go away; it really is an inflammatory imbalance more akin to asthma than a chronic infectious problem. “This is a bit of a huge paradigm shift in our field,” Dr. Wang said.
Establishing the Diagnosis of Chronic Rhino without Nasal Polyps
Subjective symptoms include nasal congestion with less obstruction, thick nasal drainage, decreased sense of smell, and facial pressure. Duration is at least 12 weeks. A nasal endoscopy can be normal, CT maxillofacial without contrast is critical.
Establishing the Diagnosis of Chronic Rhino with Nasal Polyps
Subjective symptoms include nasal congestion/obstruction, thick nasal drainage, decreased sense of smell, and rarely facial pressure but a lot of difficulty breathing out of the nose. Duration is at least 12 weeks. The same objective tools are used for diagnosis and are complementary. An endoscopy can reveal nasal polyposis.
Eosinophilic Chronic Rhinosinusitis and Allergic Fungal Rhinosinusitis
This is not a fungal infection but the body’s response to fungal elements in the nose, which causes a very robust inflammatory response. One way you can tell is in the operating room; it looks like raw honey, or some people describe it as peanut butter. It is thick and tenacious. A CT scan in advance can usually reveal the different densities and the diagnosis.
This is not common in Pittsburgh, but very common in the southeastern U.S. In the south and southeast, this is probably the most common kind of nasal polyps. It is also common in the Middle East and Southeast Asia.
Treatment for both of these used to require opening the sinuses to get the stuff out. Otherwise, recurrences were high.
Aspirin Exacerbated Respiratory Disease
This usually comes on in the third or fourth decade in people without a history of asthma or atopy. They may have previously tolerated NSAIDs. The ratio of female to male is 2:1. The initial symptom is nasal drainage. Two years later, they get asthma. The last symptom is the NSAID reaction. If you ask people with this if they get a lot of nasal drainage when they drink red wine, they will say yes. Something about the tannins make it specific for this group; it is basically an acquired metabolic condition. The exact mechanism is unknown. There is a straightforward way of diagnosing, which involves a 24-hour urine collection sent to a Mayo Clinic lab.
Treatment involves leukotriene modifiers like Singular or infusions like Zileuton. A sinus surgery can also take out the bulk of the polyps, and then patients get doses of aspirin with increasingly high doses. It is not easy to do, because initially patients have to take two tablets of aspirin a day – 650 mg of aspirin. It does tend to improve people’s symptoms.
Treatment for Chronic Rhinosinusitis
The primary goal is to reduce the inflammatory burden. For people who have CRS with nasal polyps, they can use topical nasal steroid sprays with nasal saline irrigations, oral corticosteroids, and off label Budesonide. Antibiotics have poor or no effect.
If there are no nasal polyps, they can use topical nasal steroid sprays, nasal saline irrigations, and antibiotics have a small but consistent effect. Macrolide can be used for an anti-inflammatory effect. Oral steroids and Budesonide are not recommended.
Topical Medical Therapy
In over eight randomized controlled trials, saline irrigations were found to improve quality of life, symptoms, and endoscopic scoring. They reduced acute flares.
Topical antibiotics, however, fail to consistently demonstrate benefits, therefore they cannot be recommended. Some case series have reported effectiveness, particularly in recalcitrant cases of CRS, suggesting there may be a role in unusual cases.
Topical Antifungals
There have been a lot of trials with topical antifungals. According to the International Consensus Statement on Allergy and Rhinology (ICAR), there is no benefit with potential harm and cost.
On the basis of available literature, there is no evidence to support the use of systemic anti-fungal treatment.
Endoscopic Sinus Surgery: Creating an Open Floor Plan
Dr. Wang explained sinus surgery as taking all these little rooms – the different sinuses – and creating a big common space, or one common cavity per side. This allows drugs to be distributed in a much more efficient way.
“Surgery is not a curative thing,” Dr. Wang said. “It’s an adjunct to the delivery of topical medications.”
Steroids can help bring inflammation down, but only if they get to the places that count. When you combine the idea of topical therapy with surgery, you get a multimodality treatment for the control of chronic rhinosinusitis.
Clinical Trials
Dr. Wang shared some clinical trials. One found that sinus surgery and topical nasal steroids improved people’s quality of life that can be stained for up to five years. Another trial compared steroid irrigation to steroid sprays. Both help but steroid irrigation had a large benefit. But is it safe?
A small study looked at this and found that this mechanism for delivering steroids is still relatively safe.
Exhalation Delivery System
Newer mechanisms are now on the market, like an exhalation delivery system. One piece goes in the mouth and another in the nose. The breath carries the medication to the nose, but instead of turning down and going into the lungs like normal, it circulates back up higher into the nasal cavity, providing more nasal cavity distribution. Fluticasone is the same as Flonase, but a higher dose. It has FDA approval and is effective.
Sinuva
Sinuva is a stent that is placed in the office to help control polyp recurrences. It has a 90-day delivery, with the potential to avoid revision surgery. In the right person, it can be very effective – especially in patients who are diabetic. It gets removed after 90 days. While a big device, most people tolerate it well.
A Phase 3 trial of mometasone furoate sinus implants for people with CRS and recurrent nasal polyps found that it improved the polyp score, nasal obstruction, and ethmoid obstruction. The need for revision surgery was reduced in 61%, but it did not improve facial pain.
TEMPS = Thermogel Extended-release Microsphere-based delivery to the Paranasal Sinuses
This exhalation delivery system forms a gel when it touches the warmer nasal lining. This allows steroids to be delivered continuously over a month. It has been done in rabbit models. Research continues here at the University of Pittsburgh. EEF provided some of the funding to move this work along. Now they are applying for NIH funding.
Dupilumab
Biologic therapy is the latest treatment, with dupilumab the poster child for CRS. This monoclonal antibody blocks a specific protein receptor or cell receptor on the cell lining. It has been shown to significantly improve breathing. In patients with severe CRS with nasal polyps, Phase 3 trials found that it improved the polyps and nasal congestion. It received FDA approval.
The disadvantages are that it requires an injection every two weeks. It can unmask granulomatosis with polyangiitis, though this is rare. Polyps recur with discontinuation. This may not be the case in everybody yet but the data is not quite mature enough to give recommendations. The biggest drawback is the cost; it is $25,000-$35,000 a year.
Dr. Wang had a study published that compared dupilumab treatment to endoscopic sinus surgery for people with CRS and nasal polyps. As expected, the sinus surgery did a better job of reducing the polyps, while dupilumab was better with nasal drainage or sense of smell. Overall, they were pretty similar. This showed that while both therapies are effective, dupilumab is not for everybody and topical steroids combined with surgery are extremely effective without having a huge cost.
Mepolizumab (Nucala)
This antibody blocks a similar Type 2 inflammation. In a randomized, controlled Phase II trial, there was a significant reduction but no statistically significant change in symptom scores. It has FDA approval and will be an alternative when side effects of dupilumab take effect. There is a big benefit in specific subtypes.
More Information
If you are really interested in sinus, the American Rhinologic Society has a patient-facing website. Dr. Wang and his team have written things for it due to their desire to put clear information in a centralized place for patients to find.