Head and neck reconstruction is one of the toughest things Dr. Matthew Spector, MD, FACS, does as a surgeon. The Division Chief of Head and Neck Surgical Oncology and Microvascular Reconstruction, Director of the Head and Neck Surgical Oncology and Microvascular Reconstruction Fellowship, and Professor in the Department of Otolaryngology at the University of Pittsburgh School of Medicine, presented “Mandibular and Maxillary 3D Modeling in Head and Neck Reconstruction” for the Eye & Ear Foundation’s March 21st webinar.
When it comes to head and neck cancer, the goal is to defeat the cancer and ensure the best possible outcomes. But after cancer, what is there and what happens? Reconstructive surgery is needed to restore speaking, swallowing, facial contours, and quality of life.
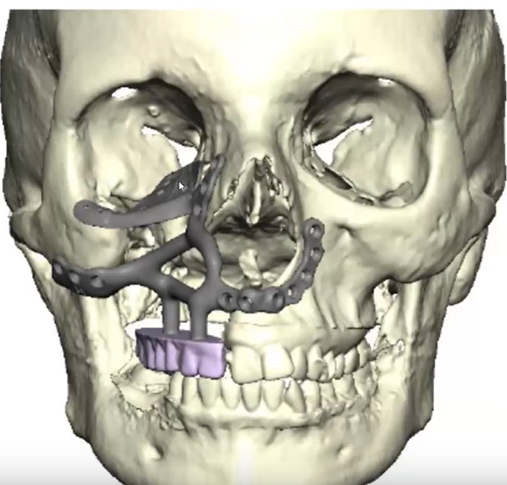
A big topic is reconstruction of the maxilla and mandible. In the last 10-15 years, new 3D modeling technology has changed the game.
Mandibular and Maxillary Reconstruction
Bony reconstruction represents some of the most complex 3D defects and are most commonly performed after cancer surgery. Patients with trauma or congenital defects also undergo this reconstruction. The mandible and maxilla are important for facial contour, speaking, swallowing, and breathing.
“Think about the complexity of your face,” Dr. Spector said. “Every day you wake up, you look in the mirror, wash your face, eat and drink, and speak to other people. These are things I think about when we’re trying to rebuild.”
Dr. Spector showed a skull picture made from a CT scan. A CT scan is run through software to build a 3D model, used to really understand the anatomy. When this patient came to him, she had already had surgery without reconstruction. She had a gap in the teeth, a depressed cheek, and a hole in the floor of the orbit. Dr. Spector had to think about all of this and how to get them fixed.
The Reconstructive Ladder
When reconstructive surgeons think about their surgeries, they employ this reconstructive ladder. The bottom rung is secondary intention, when there is a cut, gap, hole, or injury and things are left to heal on their own. The rung above that is primary intention, when these areas are sewn back together. Unfortunately, a lot of things cannot be sewn up, so the surgeon moves very quickly up the ladder to the top rung, which is free tissue transfer. In between are delayed primary closure, skin grafts, tissue expansion, and local tissue transfer.
Free tissue transfer means taking bone, skin, fat, or muscle from one part of the body and putting it in another area to rebuild the jaw or maxilla. Cadaver bone in this area or bone from a loved one cannot be used. The tissue has to be yours, so it is not rejected.
The two bones used in this reconstruction are the fibula (the bone on the outside of your leg) and scapula (Dr. Spector’s personal favorite), which is a little easier to use, patients recover a little better, and the bone shape and curvature reminds Dr. Spector of a jaw.
3D Printing vs Machining
Everything used to be machined, Dr. Spector said. This is when a computer takes a block of plastic, metal, (or whatever material), and shrinks it down by machining it. 3D printing is exactly the opposite. This additive type of manufacturing takes a model and layer by layer, is built up. It allows for making more complex shapes.
Goals of Reconstruction
When Dr. Spector talks to patients in the clinic, he asks what they want most out of reconstruction. Common things tend to include:
- Restoring oronasal separation
- Supporting the orbit
- Obtaining a healed wound in preparation for possible adjuvant therapy
- Reestablishing facial contour
- Provide a masticatory surface
- Allowing for functional dentition
Mentoring and Teaching
Dr. Spector found that mentoring and teaching residents and fellows on this kind of reconstruction was tough. He started to write papers to try to figure this out. About three years ago, he wrote a paper that still stands true today on how to rebuild an orbit. They found that the scapular bone or that shoulder bone is the best way. Patients look very normal after this surgery.
The team contracts with a company that builds 3D printing of mental plates. Dr. Spector will coordinate with one of their engineers to design how he wants the plates to go and where the projection points are. When these pieces are taken, they then figure out what fits best for each person.
Advantages of 3D Modeling
3D modeling has its advantages:
- Custom plate design
- Individual patient solutions (IPS) and virtual planning
- Decrease operative time and ultimately cost
- Education of residents and fellows
Dr. Spector shared some reconstruction examples and noted that he tells people to give themselves time to heal. When you get a knee done, you do not run out of the hospital. The concept is similar here.
The presentation ended with Dr. Spector sharing his excitement for a course he’s teaching on Advanced Mandibular and Midface Osteotomy Simulator and Techniques, on June 1. It is designed for fellows that want a little extra training before they are done; about 50 will come in and learn. This is the first year of the course.