In the Eye & Ear Foundation’s October 7 webinar, “Ocular Inflammation,” Alex Mammen, MD, started by discussing inflammation of the cornea and external eye. The Clinical Assistant Professor of Ophthalmology and Medical Director of the Charles T. Campbell Microbiology Laboratory also described several conditions that involve ocular inflammation.
In contact dermatoblepharitis, the skin around the eyes is affected. Signs include itching, redness, swelling, tearing, and mucus discharge. The condition can be caused by topical ophthalmic medications, cosmetics, or environmental substances. Reaction can be immediate (within minutes) or delayed (days to months).
Treatment involves removing the offending agent, employing antihistamines/mast cell stabilizers, or taking topical/oral steroids or immunosuppressants.
Atopic dermatitis is a chronic condition in genetically susceptible individuals with a personal or family history of asthma, allergy, or aspirin hypersensitivity. Red, itchy skin is a key feature. Causes are a delayed hypersensitivity reaction and impaired cell-mediated immunity, increased IgE hypersensitivity, or in histamine release from mast cells and basophils. Treatment is allergen avoidance, moisturizers, topical/oral steroids (for acute short-term use), or topical/oral immunomodulators (which can be used long-term).
Allergic conjunctivitis can be seasonal (caused by grass, weeds, pollen, pollutants) or perennial (caused by dust, dust mites, etc.) and affect both eyes. They may be itchy, watery, and have mucus drainage.
Supportive treatment means using cold compresses and/or preservative-free artificial tears. Systemic treatment is oral antihistamines and/or desensitization injections. Topical treatment involves antihistamines and mast-cell stabilizers, nonsteroidal anti-inflammatory drugs (NSAIDs), and judicious use of corticosteroids.
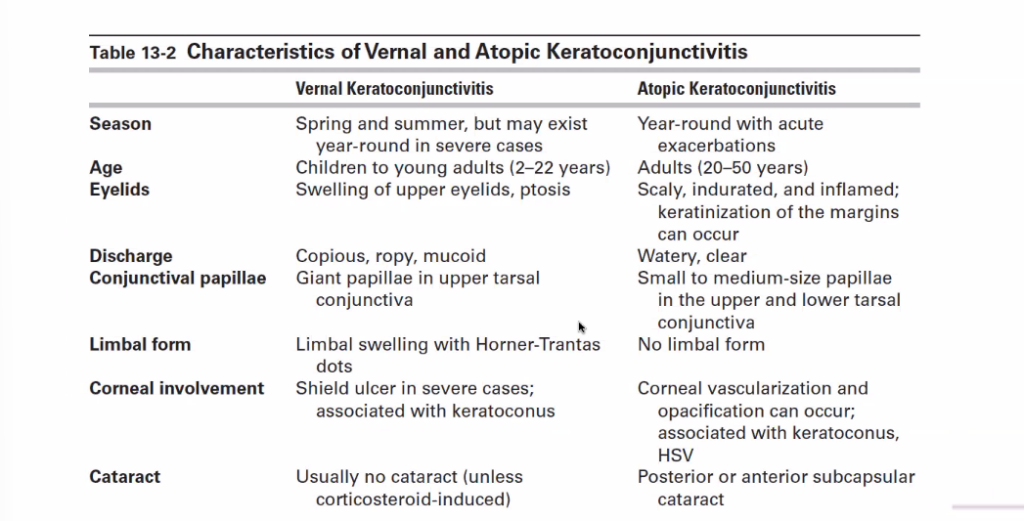
Vernal keratoconjunctivitis is a seasonally recurring, bilateral inflammation of the cornea and conjunctiva that occurs predominantly in children and young adults (2:1 male to female). Treatment is similar to above, but on a higher level.
Atopic keratoconjunctivitis is a term for adults with delayed hypersensitivity reactions and impaired cell-mediated immunity.
Cicatrizing conjunctivitis is a more severe case of inflammation that results in scarring. The surface of the eye gets clouded over by scars and looks more like the skin of the eyelids. The goal is to catch it before gets to the end stage. It can result from an allergic reaction to a drug, trauma, or environment (Stevens-Johnson syndrome), or it can be autoimmune (Lupus), or be from radiation exposure, ocular rosacea, chemical or thermal injury.
Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) affect the mouth and throat, so people can have trouble with breathing and swallowing. But the conjunctiva and oropharynx are the tissues most frequently involved. Fever, arthralgia, malaise, upper or lower respiratory tract symptoms are usually sudden in onset, with acute inflammatory, vesiculobullous reactions involving the skin and at least two mucous membranes. It can be drug-induced (NSAIDs, anticonvulsants) or from an infection (herpes simplex virus, streptoccal bacteria).
These conditions are serious; they are considered a medical emergency due to the high risk of morbidity and mortality. Patients are treated like burn patients. The offending agent must immediately be discontinued. Systemic therapy is mainly supportive and aimed at managing dehydration and superinfection. Systemic treatment with immunosuppressive agents, immunomodulatory agents, or intravenous immunoglobulins is controversial and must be used judiciously, on a case-by-case basis.
Dr. Mammen then shared several case studies. The first was a 45-year-old man who presented with left eye redness, tearing, and irritation for three weeks. There was no improvement with topical antibiotics. He was diagnosed with marginal keratitis, which has delayed hypersensitivity. The peripheral cornea is susceptible to immunologic reactions because of its proximity to limbal vasculature and conjunctival lymphoid tissue.
Signs of this condition include:
- Unilateral/bilateral peripheral curvilinear infiltrates in the superficial cornea where the lids cross the cornea
- May have epi defects or ulcerations
- Separated from the limbus by a clear corneal zone
- Circumferential progression
- Associated limbal hyperemia and conjunctivitis
- Staph blepharitis, meibomitis, acne rosacea is often present
The second case was a 12-year-old female who complained of blurry vision, foreign body sensation, and photophobia in her right eye. She had a history of chronic allergic conjunctivitis and blepharoconjunctivitis. She was diagnosed with phlyctenular keratoconjunctivitis, derived from “phlycetena,” the Greek word for blister. Signs include an elevated nodule with surrounding engorged hyperemic vessels that can become necrotic and ulcerate centrally or spontaneously involute. Pathogenesis can be a hypersensitivity reaction to an antigen of bacterial origin, like staphylococcus aureus in the U.S., or M. tuberculosis in developing countries.
Antibacterial treatment consists of eyelid hygiene, ointment to the lid margin, and topical antibiotics initially. Anti-inflammatory treatment could mean prescribing topical corticosteroids. Treating the blepharitis means eyelid hygiene, warm compresses, and oral doxycycline (100 mg daily).
A third case was a 72-year-old female with left eye redness, pain, tearing, photophobia, and decreased vision. She had a history of rheumatoid arthritis. She was diagnosed with peripheral ulcerative keratitis, a crescent-shaped peripheral corneal ulceration with an overlying epithelial defect. Patients with this may have an adjacent infiltrate and localized conjunctival injection. Scleritis and anterior uveitis are common associated findings.
Lots of conditions can cause this, from autoimmune diseases (Rheumatoid arthritis, Sjogren syndrome) to bacterial, viral, protozoal or fungal infections, or ocular, dermatologic or other systemic conditions (carcinoma, psoriasis, leukemia).
Local treatment consists of aggressive lubrication and eyelid hygiene, topical antibiotics, topical cyclosporine 0.05%, and bandaging the contact lens. Systemic treatment means oral doxycycline, systemic corticosteroids for acute control, and additional systemic immunomodulatory agents that are often required for an associated autoimmune disease. Surgical interventions may mean cyanoacrylate adhesive, penetrating keratoplasty, lamellar keratoplasty, conjunctival resection, or tarsorrhaphy.
The last case study Dr. Mammen shared was a 54-year-old male with severe eye pain, tearing, and photophobia. He was diagnosed with Mooren’s ulcer, an idiopathic peripheral ulcerative keratitis with the absence of scleral involvement and associated systemic diseases. The pathogenesis is poorly understood, but an autoimmune reaction is the most accepted theory. It can be associated with Hep C, ocular trauma, and surgery.
Signs may be a crescent-shaped corneal ulcer that begins near the limbus and progresses circumferentially and centrally. The adjacent sclera is uninvolved, while the central edge of the ulcer is infiltrated with overhanging margins. It progresses relentlessly until the cornea is replaced by a vascularized, opaque thinned tissue leaving behind a central island.
Uveitis
Marie-Hélène Errera, MD, PharmD, PhD, Associate Professor of Ophthalmology, took over the next part of the presentation. She specializes in comprehensive ophthalmology and retina and vitreous diseases. Her research interests include ocular inflammation and the epidemiology of uveitis.
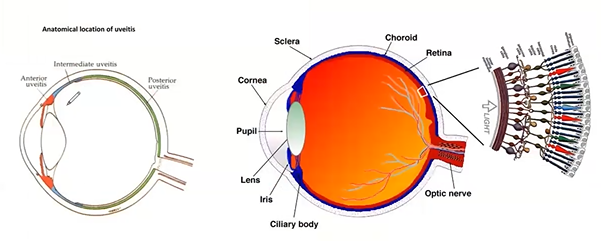
Uveitis is inflammation of the eye. It can affect the front of the eye, the intermediate part, and the back of the eye. It is associated with a systemic disease in approximately 30% of cases. Another 30% is caused by an infectious agent. In the remaining 40% of cases, the condition is idiopathic.
A multidisciplinary approach provides patient-centered care and may lead to faster, more streamlined communication between departments, potentially reducing the time to diagnosis and treatment. This is important when addressing ophthalmic conditions – particularly in the case of ocular findings with which patients are likely to have an underlying systemic disease, Dr. Errera said.
Collaborations are done with the Departments of Rheumatology and Pulmonology, imaging for diagnosis and treatments, Labs like the Campbell Lab, and imaging and immunology research. In a rheumatology combined clinic, more patients are diagnosed with a cause for the uveitis, and more patients are able to transition to steroid-sparing therapy, if needed. Corticosteroid doses can also be tapered more quickly.
Last month, UPMC Rheumatology launched a dedicated Center for Sjogren’s Disease Treatment and Research. It is run by Dr. Rachel Gordon.
There is also a monthly sarcoidosis multidisciplinary conference, where complex patients are discussed.
Sarcoidosis is a condition where the retina has lesions (along with the skin). This can affect vision.
Anterior uveitis is associated with many etiologies. The most common is seropositivity for human leukocyte antigen B27 (HLA-B27), accounting for up to 50% of non-idiopathic anterior uveitis. It can be isolated or associated with systemic inflammatory manifestations: seronegative spondyloarthropathies (ankylosing spondylitis & psoriatic arthritis) or inflammatory bowel disease.
Cytomegalovirus retinitis can also be the result of infections (not just autoimmune or inflammatory).
Dr. Errera shared an example of a six-year-old who was seen at Children’s Hospital with bilateral inflammation of both eyes. Several physicians collaborated on the diagnosis and treatment. Ocular samples were sent for lab analysis, a collaboration with infectious diseases with hematology. With the child under sedation, there are different options. A sample can be taken for a biopsy.
Dr. Anthony St. Leger’s immunology lab creates an aqueous humors bank for cytokines analysis. When there is enough volume from samples, some are sent to the lab if the patient has agreed to be part of the research. Cytokines are important proteins that act as chemical messengers in the human immune system, signaling cells to fight and other functions. This research is used to try to better understand the immune mechanisms of uveitis.
Ethan Rossi’s lab published recently with the uveitis clinic a paper entitled, “Label-free imaging of inflammation at the level of single cells in the living human eye.” Dr. Rossi uses an adaptive optics ophthalmoscopy to image the retina and look at extremely small cells. Everything can be magnified, even the vessels. Retina cells can be viewed individually. This powerful device allows physicians to see things they normally cannot with the routine imaging system used for the retina.
Ocular syphilis is a sexually transmitted infection that can affect the retina and optic nerve. Fluorescent angiography is a routine test used in the clinic to try to better detect the inflammation infection. A blood test is done, though the infection is often visible on the patient’s hand. A referral is made to infectious diseases for the final diagnosis of syphilis and treatment, because this can lead to blindness.