There are two main parts to Matthew Spector’s research. The Division Chief of Head and Neck Surgical Oncology & Microvascular Reconstruction, who has a MD and FACS, said in the Eye & Ear Foundation’s November 8th webinar, “The Rehabilitation of Head and Neck Cancer Patients,” that one is to make cancer cures better whether it is to develop a genetic test or refine a surgical technique. The other is the rehabilitation, and what life is like after cancer. It is one of the main reasons why he came to the University of Pittsburgh and UPMC, where he is building out the reconstructive or rehabilitation practice.
“I got lucky when I came here,” he said. “There’s such a great program here already. So, I had to move the little few pieces around, but all the parts were there, and we’re continuing to build.”
Free Flap Basics
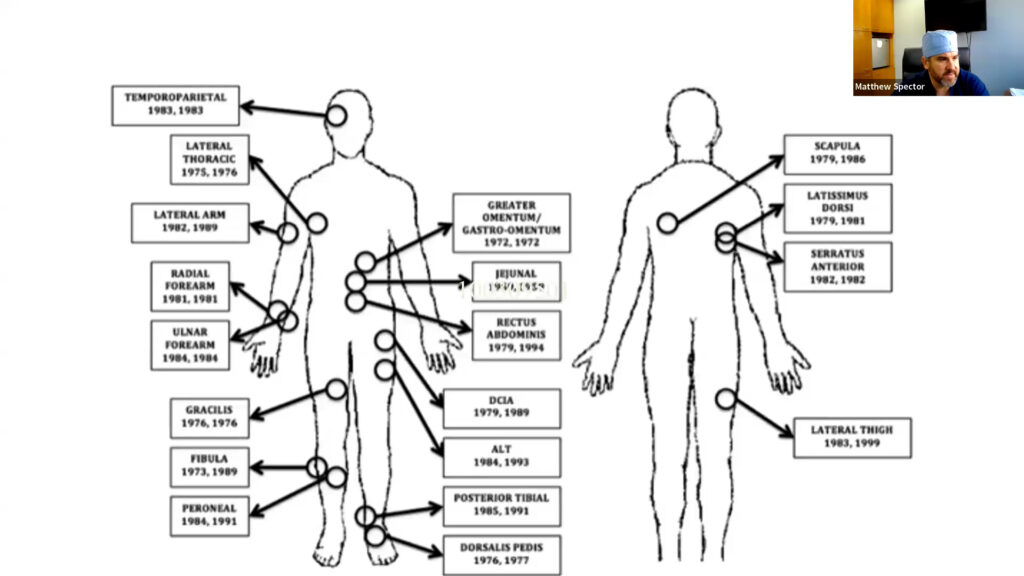
The presentation started with a description of free flap reconstruction. This is autologous (from self) tissue transfer/transplantation of tissue (skin, bone, muscle, fat, etc.) from one site of the body to another to reconstruct an existing defect.
The most common site is the forearm. The artery and vein are harvested and then hooked up underneath a microscope to the new location, where it becomes a living breathing part again.
In terms of a good or functional outcome, rehabilitation starts in the beginning.
This kind of reconstruction has come a long way since 1976. Now it is a team-based surgery that takes less than eight hours for the entire case, with reconstruction taking less than four hours. Recovery is quicker. “If you looked at my specialty, 50% of surgeons stopped doing the reconstructive part because it was too tiresome,” Dr. Spector said. The team-based approach has a mean reduction in operative time of two hours and lower fluid requirements of greater than one liter. At UPMC, team-based surgery has helped show that there are better outcomes.
Reconstructive Consideration
When Dr. Spector meets with patients in the clinic, there is a lot to talk about. One of the first things is he shows them different places where he has taken or can take flaps. There are many factors to consider when it comes to reconstruction. What is the defect? Is it fat, muscle, bone, or fascia? What are the reconstructive needs, in terms of volume/area, long pedicle, or tissue type? The goal is to maximize the functional outcome and minimize donor site morbidity and take into account patient preference and socioeconomic means.
Dr. Spector meets a lot of patients that have a very important tattoo, which means excluding or including a specific site. In general, there are too many choices and options, which can be tough. He always tells the fellows and residents he teaches to talk to their patients. This means taking a detailed history and asking patients about their occupation, hobbies, exercise preferences, prior injuries, and handedness. A physical exam should also be performed, in which tissue thickness, elasticity, scars, and tattoos should be noted.
Dr. Spector wants to know where patients are going or what they want to do in the future or what they were doing that they want to do again. Once he gets a sense of the person and their expectations, he can give expectations from his die on what needs to be done to and what things will look like.
Once the site has been selected and there’s a plan, the rehabilitation team gets involved. Rehab is always done after surgery. It is sometimes the hardest thing to explain because of expectations around surgery being scary, and people do not do a good job of talking about the next step in the process. They have started to include a little bit of it in the pre-visit, but do not always know what they will find or how things will work out with surgery, so it is a gray area.
Once the team has done the best reconstruction they can possibly do, the patient goes to the UPMC Head & Neck Cancer Survivorship Clinic. Patients have access to a speech-language pathologist, physical therapist, occupational therapist, and nutritionist, along with receiving a comprehensive evaluation and treatment planning. Since some patients do not live or work in Pittsburgh, networking is done to ensure they have support resources in their community. Marci Lee Nilsen, PhD, MSN, RN, CHPN, FAAN, Director of the Survivorship Clinic, has branched out and is trying to make this happen at other sites. The main hub might be Pittsburgh, but how can care be spread throughout SW Pennsylvania, Ohio, and West Virginia to reach more people?
Physical Therapy
Long term morbidity is best mitigated by physical therapy. Here are some areas followed by what needs to be worked on:
- Radial forearm free flap: grip strength, sensation
- Fibula: balance, foot dorsiflexion
- Subscapular System: shoulder strength and range of motion
PT begins 2-4 weeks after surgery once it is confirmed there are no limitations based on the wound. It typically lasts for three months. PT helps patients focus on strengthening donor site abilities as opposed to focusing on disabilities.
There are many handouts and resources for patients to start PT quickly. Exercises could be as simple as watching TV at night with family and using a squeeze ball. PT can be tailored depending on the patient’s needs. PT is recommended to about 90% of patients, but only 50% actually follow through. Maybe patients are getting better on their own and the team does not need to intervene, but these types of resources are where people make the most gains.
Variability of Outcome
Everyone is a little bit different when it comes to functional outcomes. This is included in the pre-counseling phase. Dr. Spector will show patients what their scar might look like after. Variability is difficult to predict, but Dr. Spector is trying to standardize the approach for all. Another difficulty is the inability to predict how things heal. “Part of the point of rehab is to know that it is unbelievably important,” Dr. Spector said. “Patients almost always get better over time. Sticking to the plan can really help.”
Nerve Reconstruction
Surgeries used to take so long just to take out cancers and rebuild things; it was difficult to spend time tweaking everything to make it perfect, especially with other things to worry about like the heart, lungs, and fluid shifts. Now with a 4–6-hour surgery, patients wake up and are sitting in a chair the afternoon after surgery. Because of this, it is possible to spend more time thinking about how to optimize reconstructions. Nerve reconstruction has been underrepresented, but we will see more of this in the future. Dr. Spector hopes that patients start to bring these things up.
Breast reconstruction, for example, has undergone incredible growth over the past 10 years. The same thing is done, in which skin and fat are taken to rebuild breast tissue for women after breast cancer surgery. Before, there would be no sensation but now they are starting to sew in nerves in that tissue to get them to regenerate so that there is feeling there. Dr. Spector knew he would be able to find similar things with head and neck cancer reconstruction.
Tumors of the cheek can involve nerves to the face. If part of the tongue is taken, sensation and taste can be lost in that area.
Parotid Reconstruction Principles
- Restoration of the facial nerve for ocular protection, oral competence, and facial symmetry
- Volume replacement to optimize cosmetic result
- Color match to surrounding skin
Dr. Spector wants to make sure that patients can move their eye, blink, swallow, and speak. For a long time, people were taking a piece of the arm and using that as the best piece of skin, which means a big scar on the arm. Patients can also have issues with their hand. Is this the best site? A study was designed to figure that out.
Volume of Parotid Defects
In a cross-sectional study of 276 patients who underwent full body imaging for melanoma, flap donor sites included parascapular, rectus, latissimus, lateral arm, anterolateral thigh, and radial forearm free flap. Parotid volume was calculated including a total parotid and superficial parotid defect.
A number of different sites were found to be good ones for this, the best one being from the back, called a periscapular flap. Dr. Spector likes the ability to hide an incision on someone’s armpit crease, back, or underneath clothes. “As you talk to people, you’ll find out these scars do bother them,” he said.
In women, they found that periscapular flap proportion was higher, whereas men had a little bit of a smaller chance of having a match but had other sites that could be used. It might be different by gender, BMI, or weight; this is something Dr. Spector talks to patients about. Parascapular flaps may more closely reapproximate volume reconstruction in parotid defects.
Color Match of Parotid Defects
- Cross sectional study of 132 pts with parotid or neck defects
- Multiple time points were used when available
- de2000 – is most frequently used in graphic arts applications and is the industry standard for computational color differences
Colors tend to match over time and get better over time in all flaps. MSAP followed by parascapular and lateral arm flaps have the best color match for parotid and neck defects. People tend to be paler in their legs than in the upper extremities.
Dr. Spector counsels people about the different strengths and weaknesses of different sites, and tries to express the benefits of this and downside of that, so that they can pick the best option.
Oral Cavity Reconstruction Principles
- Obliterate the volume in the oral cavity
- Maintain premaxillary contact
- Optimize the residual “finger function” of the tongue
- Maintain movement of secretions from the anterior to the posterior aspect of the oral cavity
- Optimize sensation of the remaining native tissue and the revascularized free tissue transfer
How does sensation matter? What can be done with the nerves of the tongue to help the tongue rehabilitate, and what does this look like? In a paper published two years ago, Dr. Spector hoped to show that if he took the time to hook up nerves to the tongue, he could get a better functional outcome. He was able to show this, with patients reporting they could swallow, speak, and eat better. He pointed out that people do not realize there are a lot of tongue branches and nerves. The lingual nerve, for example, is not just about sensation, but taste, pressure, and temperature.
In a cohort of 84 patients, one group had their nerves hooked up, while the control group did not. Turns out, it works. He asked patients questions, but it was all about asking the right questions. If he asked how someone was eating, they would say, “Ok.” But if he asked what type of solid foods they ate, then they get into the details. The neurotized group did extremely well and was able to have an excellent range of liquids without a feeding tube. Almost all of them could drink almost any liquid in any consistency of speed. Their range of solids was also good, as was their speech understandability.
Flap Choice in Low Volume Tongue Reconstruction
- Cross sectional study of 39 pts who underwent subtotal hemiglossectomy or total hemiglossectomy
- U of Wash Qual of Life (UW-QOL) survey and Eating Assessment Tool (EAT-10) greater than six months post operatively
- Flap donor sites included radial forearm, ALT, ulnar, and AMT
The same study was repeated with different groups of patients, looking at quality of life. The patients in the nerve grafting group had better reported swallowing. “It was very striking and kind of changed how we look at nerves for me and my team,” Dr. Spector said. “It is not standard everywhere else.”
Summary
- Rehab begins with preoperative counseling around donor site selection
- Early physical therapy and survivorship clinic engagement yields better results
- Nerve rehab during surgery allows for improved outcomes
“I can’t stress it enough,” Dr. Spector said. “Nerve rehabilitation is going to be an unbelievable part as we go forward to understand how we take care of patients.”