Chronic rhinosinusitis is probably one of the most common complaints that Dr. Eric Wang sees in his practice and in his world. “Even though we call it one thing, it probably is a variety of different pathologies that run into the same idea and topic,” he said in the Eye & Ear Foundation’s March 26, 2025, webinar, “Etiologies of Chronic Rhinosinusitis.”
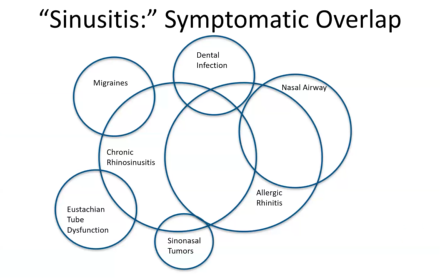
Chronic rhinosinusitis, or CRS, does not have very specific symptoms; there is a lot of overlap with many other conditions, including migraines, dental infections, nasal airway, allergic rhinitis, eustachian tube dysfunction, and sinonasal tumors. As a result, there is crossover with dental and neurology colleagues.
In fact, it is difficult not just for physicians but also patients to differentiate between the conditions that mimic sinusitis. The first great mimicker is headaches or facial pain.
Headaches
Headaches can be confusing because the predominant symptom is facial pain. Migraines can actually cause increased nasal drainage and nasal congestion.
Different types of headaches include tension, migraine, sinus, cluster, TMJ, neck, hormones, and stress. When pain is the predominant symptom, patients often have clear CAT scans to show the sinuses have no inflammation.
Midface Segmental Pain
Midface segmental pain is bilateral facial pain without evidence of sinusitis. In a Korean National Survey of 31,999 patients, prevalence was 0.59%. Risk factors are chronic rhinitis and stress.
There is a lack of correlation between facial pain and CRS. In one study of 73 patients with CRS and facial pain, there was a lack of correlation between the location and severity of the facial pain. In a second study, 78 patients out of 203 had CRS and facial pain, but no correlation was found.
Rhinogenic and Non-Rhinogenic Headaches
About 16-20% of CRS patients report facial pain. Forty percent of facial pain persists after treatment with resolution of sinusitis on CT or endoscopy. Rhinogenic facial pain, defined as facial pain that resolves with treatment, was associated with a 97% positive CT.
Dental and TMJ Pain
Tooth roots go up through into our midface. That same area is where we often have pain and discomfort. Dental pain is probably one of the most common mimickers of CRS and can last for a long time. The two are not entirely separate. There are conditions where the tooth is infected or causing pain, and it also causes sinusitis. But there are other conditions where the dental or nerve pain itself is present without sinusitis. It can be difficult to distinguish between these.
Because orthodontics is such a common intervention in the United States, another great mimicker is pain in the jaw joints called the TMJ joints. This pain can spread to the muscles that give our chewing ability, which are behind the sinuses.
Chronic Rhinitis and Rhinosinusitis
This is another area where symptoms overlap: nasal congestion/obstruction, nasal drainage, decreased sense of smell, and facial pressure. It is important to separate chronic rhinosinusitis with nasal polyps from allergic or chronic rhinitis. Each is treated in a different way after the initial therapeutics are done.
Role of Facial Pain
In 479 patients who had three out of four symptoms, 45% were without CRS by CT, and 39% were without CRS by endoscopy. Eliminating pain as a primary symptom increased specificity from 37.1% to 65.1%. Comorbidities were TMJ disorders, chronic neck pain, and depression/anxiety.
“The etiology of facial pain actually coming from your sinuses is unfortunately a little less common than we would like it to be,” Dr. Wang said. “When I do find sinusitis, I kind of like it, because a lot of times I do help the patient. It is much more difficult when I can’t.”
Recurrent Acute Sinusitis
If a patient has four or more episodes without symptoms between episodes, they might have recurrent acute sinusitis. It can be viral or bacterial. Double worsening is a sign; this is when they are worse, get a little better, and then get a lot worse. These patients respond very well to antibiotics.
Sinusitis
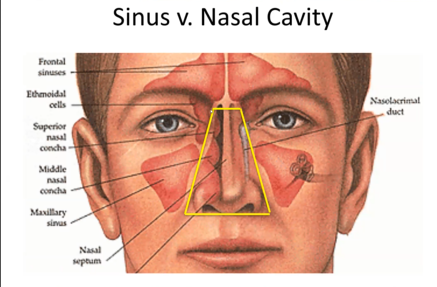
In this photo, the nasal cavity is outlined in yellow. The sinuses are the exterior pink structures. Symptoms overlap a lot, but the key question is, is there really inflammation in the outside places?
What is Chronic Rhinosinusitis?
Chronic rhinosinusitis is 12 weeks or longer in duration. The four “cardinal symptoms” are drainage, blockage/congestion, hyposmia/anosmia, and facial pressure – not headache or facial pain. Objective findings are through a CT scan or nasal endoscopy. Chronic rhinosinusitis (CR) is inflammation that mimics infectious symptoms but does not equal infection.
Establishing the diagnosis of CR without nasal polyps means having the subjective symptoms of nasal congestion (but less obstruction), thick nasal drainage, decreased sense of smell, and facial pressure. Duration is at least 12 weeks. Objective measures are a nasal endoscopy (can be normal), and a CT maxillofacial without contrast.
CR with nasal polyps have the same subjective symptoms as CR with nasal polyps, though perhaps a little less facial pressure. The same objective measures are used to diagnose.
What causes CR? Sometimes teeth, as in odontogenic chronic rhinosinusitis. With maxillary molars in the maxillary sinus, an infection at the root can infect the adjacent sinus. The sinus itself has no inflammation, but the tooth can drive inflammation into the sinus.
A mucous retention cyst sometimes occurs in people who have bad teeth, but it also sometimes just happens for no apparent reason. If scans were done on 100 people whose teeth feel totally normal without any nasal symptoms, about 15 of these cysts would be found, so it is pretty common, but in itself not a problem. It is rare to do anything about them.
Odontogenic sinusitis limited to the maxillary sinus is when most of the sinus is swollen but still open. This person needs their tooth to be taken care of, not sinus surgery. As long as the tooth is corrected, nothing else is needed.
Ascending odontogenic sinusitis is when sinusitis last longer. The infection has spread outside the cheek sinus and spread to the ethmoid sinuses near the eye and to the frontal sinuses in the forehead. When it spreads outside, unfortunately the vast majority of the time sinus surgery is required to clear the chronic inflammation and infection before a complete resolution of symptoms. People tend to get a little better with antibiotics or drainage. The pressure goes away but then it comes back in 3-4 weeks, a classic pattern.
Symptoms include purulent drainage (sometimes predominantly post-nasal drainage, with a foul smell most common), facial pressure, and frequently absent from dental pain. Dental cysts/tumors and dental implants and sinus lifts can cause infection and CR.
Secondary CRS, or odontogenic sinusitis, is treated with sinus surgery followed by oral antibiotics as well as dental interventions.
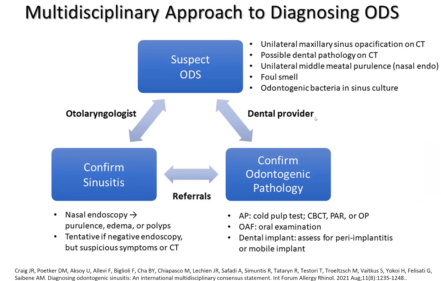
A multidisciplinary approach to diagnosing odontogenic sinusitis is shown on this paper done by Dr. Wang’s colleague at Henry Ford. Endodontists are helpful to work with to confirm the sinusitis portion as well as the odontogenic portion to confirm this etiology. “We’re very fortunate in the Pittsburgh area to have some really wonderful dentists to allow us to work in a collaborative manner,” Dr. Wang said.
Inflammatory Imbalance in CR
In CR with nasal polyps, there is a 0.4-2% prevalence, a high symptom burden of nasal congestion, increased rhinorrhea, decreased olfaction, recurrence of polyps, and Type 2 inflammation with eosinophilia (an allergic kind of inflammation). There is a balance between inflammatory signals and regulatory signals (cytokines) in the nasal cycle with normal sinus inflammation. In CR, there is dysregulation and imbalance between inflammatory signals and regulatory signals. “We can pretty safely say now they are not infections or chronic infections but inflammatory imbalances.”
Air Pollution and CR
Air pollution is correlated incidence and prevalence of CRS, with a worse severity of symptoms, and changes on histopathology. If there is more air pollution in an area, there is a higher incidence on how often CR occurs.
Air pollution can disrupt the epithelial barrier and may activate Type 2 inflammation. Some of these same markers increase because of this disruption. “We are beginning to understand more can happen from things that we experience in our environment every day,” Dr. Wang said.
Smaller particles (like fine sand or human hair) have a greater negative effect on people, according to a study in the Bay Area. A study out of Nashville found that the more particulate matter a patient may have experienced by their zip code, the more tissue swelling there was.
The effect of air pollution on the sinus epithelium results in increased inflammation, increased eosinophilic aggregates (Type 2 inflammation), and increased Charcot-Leyden crystals (marker of eosinophilia).
Air Pollution in Western PA
Socioeconomic status is associated with increased exposure to air pollution. Our air quality has improved tremendously over the past 30 years but is not perfect yet, Dr. Wang said. By most metrics, we still have a little bit higher degree of air pollution than a lot of areas.
A study here that has been published and peer reviewed looked at the population of sinus patients and tried to classify them by zip code to look at their particulate matter and black carbon indexes. In this cohort, they were unable to find a clear driver of particulate matter and air pollution indexes and sinusitis. The challenge is that the area is a bit more homogeneous. They did show, however, more severe sinusitis.
Viruses and CR
In patients with CRS with nasal polyps, 80% had positive viral screens. Only 20% did in patients with CRS without nasal polyps. The SNOT-22 (Quality of Life) survey was higher with a positive viral screen. Coronavirus was most commonly detected.
Secondary CRS: Fungal Ball
All of us live with fungus in our nose, but in some, it starts to proliferate and grow. Symptoms include purulent drainage, facial pressure, and unilateral nasal congestion.
Sphenoid Fungal Ball
Symptoms are headaches at the top or back of the head and post-nasal drainage.
Eosinophilic CR Allergic Fungal Rhinosinusitis
This involves nasal polyposis and thick eosinophilic mucin that is like raw honey in its consistency; it is very sticky. There is less of this in the northeast, but in the southeast and all the way to Texas, is incredibly prevalent. The Middle East is another hotbed.
With this, three inflammatory drivers are strongly unregulated. There is no good reason why fungus should be driving these inflammatory markers. A colleague looked into decreased histatin, whether it is a deficient Type 3 immune response. Patients with this allergic condition have severe asthma.
Duplumab can help people with this histamine dysfunction and stop inflammation; it is one of the newest monoclonal antibodies.
Aspirin Exacerbated Respiratory Disease
This tends to start in the third or fourth decade where there is no history of asthma or atopy. People with it may have previously tolerated NSAIDs. The ratio of females to males with it is 2:1. They tend to have a history of worsening nasal symptoms when drinking red wine. The initial symptom is rhinorrhea, followed by asthma two years later. The last symptom is a NSAID reaction.
The exact mechanism is still unknown. It is considered an acquired metabolic condition. The preferred diagnosis is through a 24-hour urine collection, with the alternative being random collection. Beware of systemic mast cell disease or 5-lipo-oxygenase inhibitor therapy. Normal levels equal 104 ng/ml or less.
Medical treatment involves leukotriene modifiers and is an area of active investigation for biologic therapy.
Current Research
Dr. Wang shared some exciting things going on in his group. One of them is a Mepolizumab (Nucala) study. This is an anti-IL-5 antibody that’s being used in a randomized, controlled Phase II trial. Forty subjects with CRS and nasal polyps refractory to steroids (polyp grade 3 and 4) were split into two groups. One group is the treatment arm, the other is the placebo arm. They received two IV administrations 28 days apart. Results at two months showed that 12 out of the 20 treatment patients had reduced polyps, and 1 out of 10 placebo patients had reduced polyps, with no statistically significant change in symptom scores.
Another project is TEMPS: Thermogel Extended-release Microsphere-based delivery to the Paranasal Sinuses. This is clever in that at low temperatures, this is a liquid, but when it gets to body temperature, it becomes a gel. In that gel, small microspheres of a drug can be embedded. This can vary from steroids to things that might restore that barrier and reduce an inflammatory response. This is still in preclinical models but is an exciting avenue of helping people without medication.
Something they are starting to dive into now and are looking for some help as they move forward is biologic therapy. It is extremely effective but also very expensive. They want to identify before trying on someone whether they can predict who will respond to the therapy and who these people might be. Will they have persistent symptomology over time? Right now, they are working on the initial banking criteria for this. The goal is to be able to help people decide which is the right intervention for them and predict who will have a great response to therapy.
In addition to Dr. Wang, Dr. Carl Snyderman, MD, MBA, and Dr. Garret Choby, MD, are part of the UPMC Division of Rhinology and contribute to the great work being done. To make an appointment, call 412.647.2100.