The Charles T. Campbell Ophthalmic Microbiology Laboratory is one of only a handful of microbiology labs remaining in the country that focuses on the eye. Alex Mammen, MD, Clinical Director, Eric Romanowski, MS, Research Director, and Jonathan Mandell, PhD, Clinical Laboratory Manager, presented at the September 12th Eye & Ear Foundation webinar, “Eye Infections: Clinical Testing and Related Research.”
The Campbell Lab
The Campbell Lab is on the second floor of Mercy Pavilion, room 2.431, near the elevators going to the rehab and low vision areas. The research division of the lab is located on the 8th floor of the Mercy Pavilion. Its mission comprises the clinical diagnosis of eye infections, federally, industry, and privately sponsored research, and education. Its namesake was born in 1885 and founded a Pittsburgh water transportation company in 1920 and Campbell Transportation in 1930. The Campbell Lab opened in 1973 supported by Charles Campbell and his wife Estelle; he died at age 90 two years later.
The Lab has had many different lab directors, with the most recent one, Regis Kowalski, MS, M(ASCP) serving for over 45 years. Robert M. Q. Shanks, PhD, is now the Executive Director. Alex Mammen, MD, is the Clinical Director. Eric Romanowski, MS, is Research Director, and Jonathan Mandell, PhD, is Clinical Laboratory Manager. Other members of the team include Vishal Jhanji, MD, Associate Medical Director; Deepinder K. Dhaliwal, MD, LAc, Associate Medical Director; and Tara Barnes, BS, Clinical Lab Technician.
Eye Infections
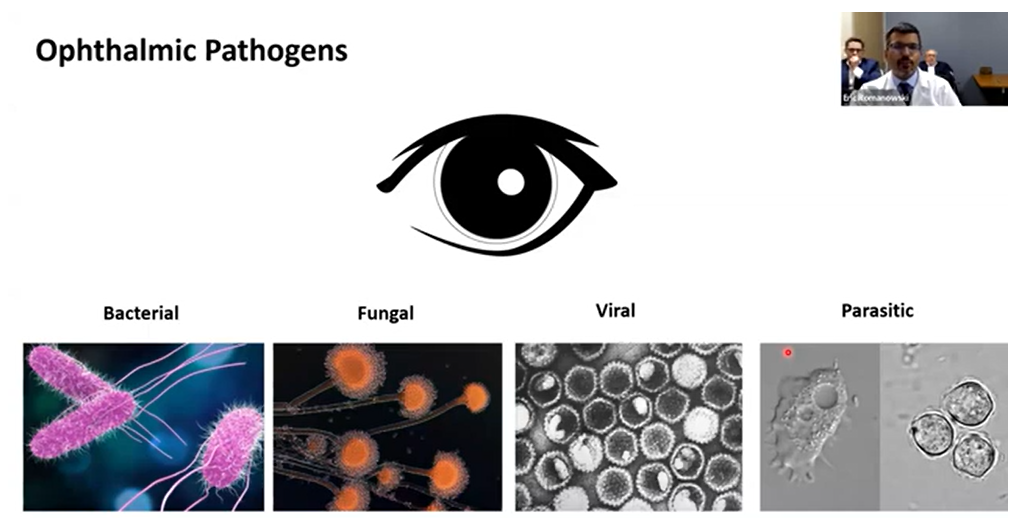
Any tissue, fluid, or space in or around the eye can get infected. The focus of this webinar was on infections involving the cornea, or the “windshield” of the eye. Ophthalmic pathogens include bacterial, fungal, viral, and parasitic. Bacterial infections can be associated with contact lens wear and are the most common cause of corneal infections in our region. Fungal infections are more common in humid areas closer to the equator, but Pittsburgh does get some. In general, these infections take longer to treat and respond to therapy. As a result, the course of treatment is longer, and vision recovery subsequently can take longer.
Herpes simplex virus keratitis is one of the more common viral corneal infections. Though rare, the most common parasitic corneal infection is caused by Acanthamoeba. One Acanthamoeba patient wore rigid contact lenses and washed them in tap water. She required a long course of drops and surgery and has had two corneal transplants so far due to complications associated with the infection.
Clinical Testing
Physicians have the opportunity to directly sample the eye they think is infected and submit it to the lab. There are largely two different types of bacteria: Gram-positive or Gram-negative, which respond differently to different classes of antibiotics. Rapid diagnostics can be provided if organisms can be identified by staining and microscopy and help to guide therapy. Swabs are also used for ophthalmic cultures and PCR-based diagnostic procedures.
The Lab also performs antimicrobial susceptibility testing. This involves testing a specific battery of antibiotics based on whether the sample is Gram-positive, Gram-negative, or from a patient with conjunctivitis, keratitis, or an infection of the inner eye, etc. Susceptibility is determined by the concentration of the antibiotic needed to inhibit the growth of the isolate. These findings are important to help the physician determine the best course of action for the patient.
All results are shown in EPIC in the patient’s chart. This is how the Lab communicates results back to the physician and patient.
Research
Lab Director Dr. Shanks could not participate in the webinar as he was on his way to Chicago to present some of the Lab work at a national meeting. His research interests include:
- Bacterial corneal infections – determining bacterial factors that influence pathogenesis using molecular genetics and ‘omics approaches
- Development of molecular biology tools – making DNA-based tools to study opportunistic pathogens
- Corneal wound healing – impact of bacteria on corneal wound healing
- Antimicrobial therapy – developing alternative antibacterial strategies like predatory bacteria for antibiotic resistant pathogens
- Drug delivery to the eye – the Lab has developed a system to deliver biologics to the ocular surface and has used this with models of dry eye and ocular surface damage
The research mission of the Campbell Lab is to:
- Investigate the basic mechanisms of eye infections
- Evaluate new and current antibiotics for use in the eye – lab testing, animal models
- Develop and evaluate new antivirals for viral pink eye – adenovirus (no treatment available)
- Responding to ophthalmic public health emergencies – rare
Outbreak
In February-March 2023, there was an outbreak of extensively drug-resistant Pseudomonas aeruginosa (PA) associated with Artificial Tears. At least 81 cases were reported in 18 states. Four patients died, 18 developed eye infections, and four underwent removal of infected eyes. The outbreak was traced to contaminated over-the-counter unpreserved multiuse bottles of Artificial Tears imported from India and purchased online.
The bacterium responsible for the outbreak was extensively drug-resistant, or XDR, and was resistant to the antibiotics typically used for treatment of keratitis – which was quite a shock. Multiple classes of antibiotics are used in ophthalmology and work by different mechanisms:
- Fluoroquinolones (DNA interference)
- Cephalosporins (bacterial cell wall)
- Aminoglycosides (protein synthesis)
PA is a highly versatile, rod-shaped bacterium found widely in the environment, particularly in soil and water. This Gram-negative bacterium is a significant opportunistic pathogen and one of the leading causes of hospital-acquired infections. Gram-negative means it has a double-membrane structure, making it intrinsically resistant to many antibiotics.
PA is a major cause of lung infections, including pneumonia, especially in patients with cystic fibrosis (CF), chronic obstructive pulmonary disease (COPD), and those on mechanical ventilators. It can cause severe and rapidly progressive eye infections, especially in contact lens wearers.
PA keratitis is the second leading cause of corneal infections at the Vision Institute – about 18% of all corneal infections. It is the leading cause of contact lens-related eye infections. Three antibiotic eye drop treatments are available; one is commercial, and two must be prepared in a specialty pharmacy.
Antibiotic resistance occurs with efflux pumps and factors made by the bacteria. Typically, there is not much resistance in PA eye isolates.
The isolate that caused the infection is of a type never found before in North America. It was resistant to several antibiotics, including those used in ophthalmology. It was susceptible to one used for pneumonia and urinary tract infections, however – cefiderocol. Could this be repurposed as eye drops to treat this XDR PA corneal infection?
Cefiderocol
Otherwise known as Fetroja (cefiderocol for injection). It was FDA-approved in 2019 for Gram-negative UTIs. It is given by IV infusion and never tested for use as an eye drop. It is rationally designed siderophore cephalosporin; it tricks the bacteria into taking up the antibiotic and is therefore called a “Trojan Horse” antibiotic.
The Lab did antibiotic testing of many PA isolates in its collection, including the outbreak strain from the CDC. The results were highly promising with 100% of PA isolates being susceptible to cefiderocol.
All concentrations of cefiderocol were non-toxic and well tolerated in a rabbit model, so 5% cefiderocol was chosen for the efficacy study. The results suggested that this drug could be a safe and effective topical treatment for keratitis caused by XDR PA.
Preservatives
Most multiuse eye drop formulations contain a preservative to prevent contamination by microorganisms, but the Artificial Tears associated with the outbreak did not include a preservative. The Lab determined whether a preservative could have prevented the XDR PA-associated eye infection outbreak. Was there something different about the outbreak isolate that would have made it resistant to common preservatives used in eye drops? The study compared the outbreak isolate to other PA strains for effectiveness of common preservatives alone and in preserved and preservative-free commercial Artificial Tears.
The conclusions:
- Common preservatives were effective in eliminating PA strains, including the outbreak strain.
- There was no difference in effectiveness with any of the preservatives tested between the PA strains.
- A preservative in the Artificial Tears may have prevented the eye infection outbreak of 2023.
This study was just published in Current Eye Research.
Future Studies
- Combination therapy using cefiderocol with Moxifloxacin or Polymyxin B to treat XDRPA keratitis – combination therapy can actually improve the efficacy of individual antibiotics and reduce the ability of bacteria to become resistant.
- Pathogenesis studies to determine why the outbreak strain caused systemic infections after ocular inoculation. The Lab is asking whether there is something special about the virulence ability of the outbreak strain, or whether it caused worse outcomes simply because it is antibiotic resistant.
Support
The Campbell Lab has received support from the Campbell Family Foundation, Bruce & Barbara Wiegand Family Foundation, The Eye & Ear Foundation of Pittsburgh, National Eye Institute grants to the Department of Ophthalmology and Dr. Shanks, and an unrestricted grant from Research to Prevent Blindness, which provided additional Department funding.