The Voice, Airway & Swallow Center has novel technology for head and neck cancer patients and is working with the UPMC Head & Neck Cancer Survivorship Clinic and speech language pathologists to implement them.
Most places, for example, do not have the novel Tongueometer, a tongue strengthening tool that utilizes an app for biofeedback and to track progress. This is in conjunction with a unique protocol involving expiratory muscle strength training that has promising data for its use in head and neck cancer (HNC) patients. The novelty is that this combination of therapeutic interventions is not very well studied as an instrument in this population.
While the Iowa Oral Performance Instrument (IOPI) is used to measure tongue strength and endurance and has been well studied, it is the combination of using it as part of a special therapeutic regimen for patients who cannot swallow after HNC treatment that makes it more novel.
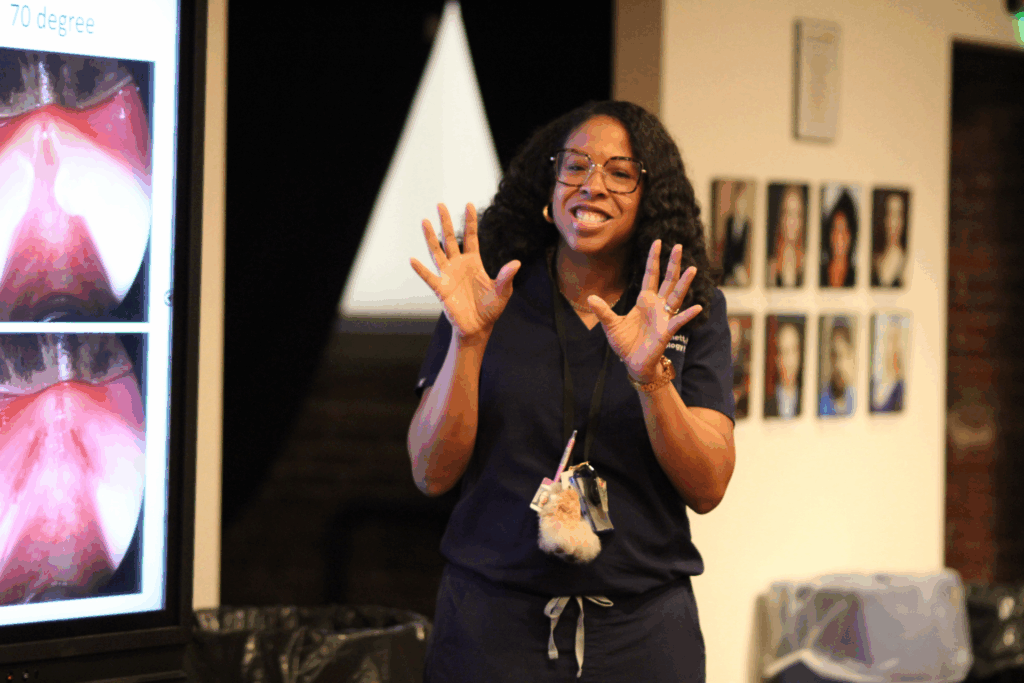
The technology that is novel in the HNC population is surface electromyography ($7000), which Dr. Stinnett, MD, Director of the UPMC Swallow Disorders Center, would like to bring to the clinic. It would be used as biofeedback for HNC swallow therapy and may help guide providers in surgical interventions for dysphagia and HNC. Dr. Stinnett and her team look forward to studying innovative protocols to manage the full gamut of patients with dysphagia.
Another thing on Dr. Stinnett’s wish list is pharyngeal manometry ($30K), which looks at muscle contractility, something that HNC patients face after treatment and is not well understood. “We’re just scratching the surface in trying to figure out how to navigate that,” she said. “This machine will help us better understand oropharyngeal as well as esophageal dysphagia in post treatment HNC patients and allow us to implement more targeted treatment plans to optimize swallow outcomes.”
Both devices provide biofeedback, which is widely known to result in better therapeutic adherence and outcomes. These modalities would allow the Swallow Disorders Center to evaluate dysphagia on a granular level, further investigate it in HNC patients, and be able to provide more tailored and streamlined treatment. It will also allow for more outside of the box thinking, “like medications to help the swallow efficacy, examining distal swallow function, looking at the esophagus in collaboration with our GI colleagues on dysmotility, and better-informed preoperative counseling with new information,” Dr. Stinnett said.
Dr. Stinnett is also interested in exploring these tools to help patients with no burp syndrome or retrograde cricopharyngeal dysfunction. In addition to providing biofeedback, surface electromyography and pharyngeal manometry can be utilized to help understand the pathology better, as well as the efficacy of non-surgical interventions. Currently, Dr. Stinnett injects the cricopharyngeus muscle with Botox, which causes the muscle to relax and allows these patients to burp. These patients continue to burp when the Botox wears off, but why? “Maybe with further evaluation utilizing these tools, we could see what is occurring functionally at the level of the muscle through the transition period once the Botox wears off. This will also help us fine tune non-invasive therapeutic interventions in this patient population,” Dr. Stinnett said.