Presenters Jillian Glasstetter, Aud, CCC-A, and Philip Perez, MD, were excited to talk about cochlear implants in the Eye & Ear Foundation’s October 31 webinar, “Expanding Access to Cochlear Implantation: Who is a Candidate Now?”
How Do We Hear?
Dr. Glasstetter, Coordinator of the Cochlear Implant Program at UPMC, started off with a basic understanding of how we hear naturally. Sound comes from the outside world, travels down the ear canal, vibrates the middle ear portion, which consists of the eardrum and three middle ear bones: hammer, anvil, and stirrup. Those vibrations then vibrate the fluid inside the cochlea, which stimulates the hair cells and auditory nerve.
Hearing with a hearing aid utilizes the same mechanisms. The difference is just that sound is being picked up through the hearing aid’s microphones. For some people, this amplification is sufficient to overcome any hearing loss.
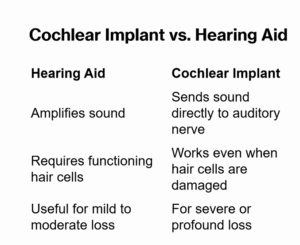
For a lot of people, however, it is not. In these cases, the sound with a hearing aid is pumped through a damaged system. “Essentially there are just not enough functioning hair cells to get a clear signal from the outside world to the brain,” Dr. Glasstetter said. You may be able to hear something, but you cannot quite understand it.
A cochlear implant bypasses all of that. It bypasses the outer ear, middle ear, cochlea, and damaged system. The cochlea houses the devices, but it is the auditory nerve that is directly stimulated.
A cochlear implant (CI) turns sound into electrical signals that the brain can understand. Sound enters a microphone in the speech processor, which converts it to a digital signal that reaches the transmitter worn on the head, sent wirelessly through the scalp. A receiver implanted in the skull turns it into an electrical signal and sends it to the cochlea. Electrodes in the cochlea stimulate the auditory nerve, allowing the brain to interpret the signals as sound.
CI Timeline
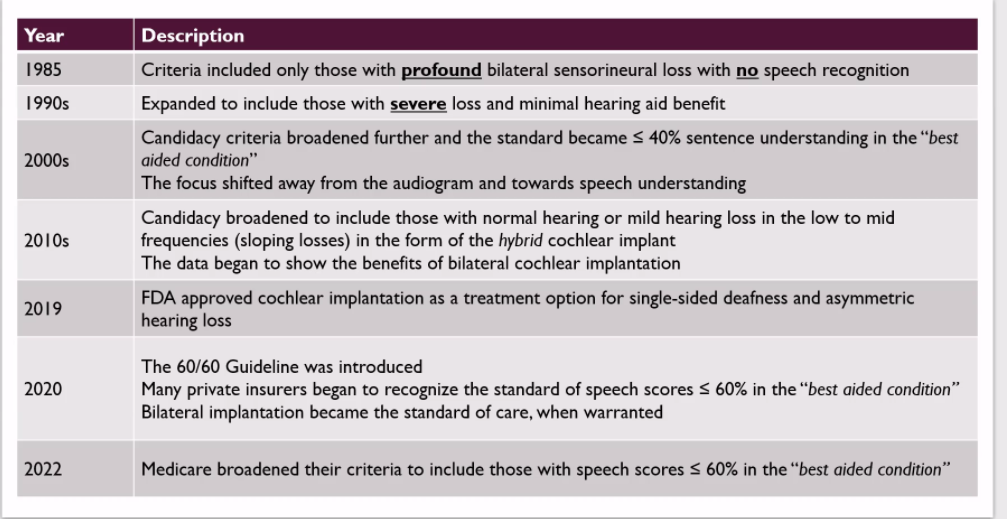
The focus of the webinar was primarily on what happened from 2010 until now. The criteria have expanded over the years. This is important because fewer than 10% of people who qualify for a CI actually receive one. Many people may not know they or their loved ones qualify. This is in part due to the historic candidacy criteria of having to have a profound or severe to profound hearing loss. “This drives a lot of the work that we do in our clinic, which is to get the word out and let people know they may qualify and benefit from a CI,” Dr. Glasstetter said.
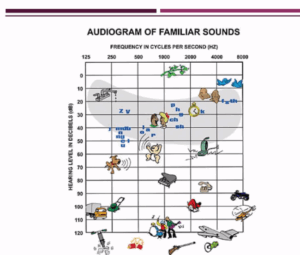
Hearing is graphed on an audiogram. The top shows frequency or pitch. The left shows low, deep pitches. The far right shows very high frequencies and high pitches. The Y axis depicts volume. As you go down the graph, sounds get louder.
60/60 Rule
The 60/60 rule is used to help determine candidacy. The first criterion is audibility: pure-tone average (500, 1000, 2000 Hz). Is it greater than or equal to 60 db in the better ear? The second is speech understanding: unaided word recognition score. Is it less than equal to 60% in the better ear? Both criteria do not need to be met; one is sufficient for a referral to have an official CI evaluation.
Daily interactions are also taken into account. If the patient experiences any of the following, they may be a candidate:
- Struggles to hear on the phone
- Has difficulty understanding others
- Withdraws from social events
- Often needs others to repeat themselves
Electroacoustic Stimulation
Another way criteria has been expanded in the last 10 years is via electroacoustic stimulation (EAS). Historically, people whose hearing tests showed they had too much hearing to lose in the low frequencies, with some detection levels falling within the normal hearing range, would have been told it was too risky to get a CI. Today, however, it has become standard of care to implant people who have hearing loss like that and accompanying word recognition difficulties.
“If someone comes to us and their speech understanding is fantastic, we won’t mention a CI,” Dr. Glasstetter said. “But if their speech understanding is poor, then it is reasonable to talk about it because someone can hear those low frequencies, but that doesn’t mean they can understand speech.”
Natural Hearing
The surgeon will always make their best attempt to preserve hearing; this is very common nowadays. It does not always happen, but it is always the goal. Surgical techniques have come a long way. The internal devices that are implanted are a lot softer, more flexible, and cause a lot less trauma than they used to.
Dr. Glasstetter’s job as an audiologist is to see what hearing is left after surgery, which hopefully is a lot. Whatever is left is used to turn the hearing device into half hearing aid, half CI. One portion goes in the ear – utilizing the acoustic or natural hearing – and the other part is stimulated with electrical hearing, or with the CI itself. This allows for a lot of improvements in sound quality.
This might be referred to as a hybrid CI, but the preferred terminology is EAS because hybrid CI refers to a specific type of internal device that is not used often anymore.
Single-Sided Deafness
Another way in which the CI criteria has expanded is by implanting people who have hearing loss on one side and normal or near normal hearing in the other. A study came out in 2019 that got the FDA on board with the benefits of binaural hearing. They started to recognize that we do need two ears to hear in many situations, and there are a lot of benefits to implanting one ear.
Common solutions for single-sided deafness include the traditional hearing aid, a bone conduction device, or a CROS or BiCROS device. The method is to take sound from the bad ear and send it to the good ear via bone conduction – either surgically or non-surgically. Note, this only allows hearing out of one ear and does not restore hearing to both.
Binaural hearing is important because otherwise, people will have:
- Difficulty telling where a sound is coming from
- Difficulty hearing in background noise
- Decreased quality of hearing (sound quality)
- Bothersome tinnitus
- Increased auditory effort – fatigue
Single-sided deafness candidacy criteria requires profound sensorineural hearing loss in the ear to be implanted, better ear thresholds between 0 and 55 db, and a word score in quiet that is worse than 5% in the ear to be implanted. The word score figure is very strict, but Dr. Glasstetter anticipates this will continue to change and broaden in the next few years. It already has, as many insurance companies are implanting up to 50-60% word scores.
Medicare does not cover CIs for single-sided deafness cases, but Dr. Glasstetter thinks this will also change. Some forms of Medicare will pay. The clinic works with a lot of UPMC for Life patients, which is a form of Medicare. They cover up to 60% speech understanding.
To recap, a lot of the audiogram is now covered when it comes to qualifying for a CI. People who have some normal hearing thresholds are getting one. This does not mean that people who do not need them or would not benefit will still be recipients. But if you are struggling and have hearing loss and have tried hearing aids, it might be worth looking into whether a CI will be beneficial.
Additional criteria takes into account considerations like:
- Hearing and HA history
- Cognition
- Family support
- Motivation
- Overall health, i.e., able to undergo surgery safely
- Appropriate expectations
You will not wake up with normal hearing. It is never going to sound as good as you remember. The goal is for it to be better than how you are hearing or not hearing now, with or without a hearing aid.
Am I Too Old to Get a CI?
Health is more important than age. From 2020-2024, the average age at implantation was 63 years old, at least 26 recipients were 80+ years old, and a 97-year-old was recently implanted!
Dr. Perez, Assistant Professor of Otolaryngology-Head & Neck Surgery, is one of three CI surgeons. Peter Santa Maria, MD, PhD, and Gregory Basura, MD, PhD, are the other two who perform one of the most common surgeries in their division. They all work with Dr. Glasstetter and her team of CI audiologists.
“It’s really miraculous that we have this technology,” Dr. Perez said. “It’s part of how I ended up in this field because it’s a wonderful gift to be able to restore somebody’s ability to understand speech and communicate with others. We love to do this, love to see the success, and really our goal is to broaden access to CIs and to keep pushing the envelope on how we can achieve greater success for more patients to live the lives they want.”
Hearing loss matters because over 430 million people worldwide have disabling hearing loss. It affects communication, independence, and mental health. It is also linked to social isolation, depression, and even cognitive decline.
CI Candidacy
CI candidacy is determined by an audiologic evaluation, which is more in depth than a standard hearing test. Pure-tone thresholds and speech recognition are tested. This involves repeating back recorded sentences done in different pitches and environments. Hearing aid benefit is also assessed. Some people looking into a CI have not been set up with the optimal hearing aid option; there are options that can still help them function at a high level with hearing aids.
A medical assessment is also done, looking at ear anatomy, overall health, and surgical feasibility.
Outcomes and Benefits
CIs provide people with a dramatic improvement in speech understanding, a better quality of life, social engagement, and cognitive health. It is a safe outpatient procedure with high satisfaction and overall is low risk with a low chance of complications.
To overcome barriers to a CI, increased education for primary care, audiologists, and patients is needed. Early referrals for evaluation along with timely diagnosis and intervention are also crucial.
“It’s our pleasure to talk to patients about this and help them get that information,” Dr. Perez said. “It’s common for us to see patients who ultimately are not quite at the point where they would consider a CI, and that’s great because they still have the ability to benefit from hearing aids and know what their hearing health is and have something to compare to down the line. They have more information about their options going forward.”
Continued Advancements
A big issue is optimizing hearing preservation. The goal is to limit anything that could cause the reduction of natural hearing. One way to do that is utilizing technology that lets surgeons monitor the function of the inner ear during surgery, getting live feedback on the health of the inner ear. Robotic assistance helps minimize any microtraumas or irritation of the inner ear caused by human tremors at the time of surgery. One such company has its headquarters in Pittsburgh.
Telehealth applications are also increasing, which will benefit people who do not live near a center. External processor programming is also advancing – both in terms of software and technology.
Summary/Take Home Messages
- CIs restore meaningful hearing when hearing aids are not enough
- Criteria are broader than ever – more people can benefit
- Safe, proven, and life changing across all ages
- Timely referral for evaluation
The final slide had this statement: “Hearing is connection, and connection is life.”
