You know how people say, “You had to be there?” That is the case with The Eye & Ear Foundation’s November 19 webinar, “Imaging for Retinal Diseases.” It is one thing to describe the different imaging modalities. It is far more effective, however, to do this by showing what each detects.
The good news is if you missed this presentation the first time around, the webinar has been uploaded to our site. In the meantime, here is a summary.
Imaging Modalities and Techniques
 After an introduction by the Department of Ophthalmology Chair Dr. José-Alain Sahel, Kunal Dansingani, MBBS, MA, Associate Professor in the Retina and Vitreous Service in the UPMC Eye Center/Department of Ophthalmology, talked about the motivation behind imaging technology. The tissue scale necessitates the development of microscopes, he said, and the most useful ones reveal relationships between anatomy (structure), physiology (function), and pathology (aberrant function).
After an introduction by the Department of Ophthalmology Chair Dr. José-Alain Sahel, Kunal Dansingani, MBBS, MA, Associate Professor in the Retina and Vitreous Service in the UPMC Eye Center/Department of Ophthalmology, talked about the motivation behind imaging technology. The tissue scale necessitates the development of microscopes, he said, and the most useful ones reveal relationships between anatomy (structure), physiology (function), and pathology (aberrant function).
In a never-ending circle, imaging provides biomarkers for understanding the effects of treatment, which leads to treatment advances that occur in parallel with imaging advances.
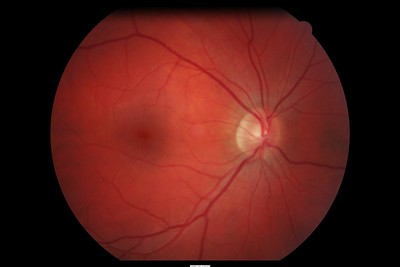
The focus of today’s presentation was on the retina, or more specifically, the posterior pole and a small part called the fovea, which is 1.5 mm in diameter. This area has a profound effect on vision.
 To view this part of the eye, color photographs are extremely useful. Other modalities involve various wavelengths of light like a 3D modality called optical coherence tomography. This provides a cross section of the fovea that’s become the gold standard. It is used daily on almost every patient in the retina clinic.
To view this part of the eye, color photographs are extremely useful. Other modalities involve various wavelengths of light like a 3D modality called optical coherence tomography. This provides a cross section of the fovea that’s become the gold standard. It is used daily on almost every patient in the retina clinic.
Light-based imaging modalities include reflectance, fluorescence, and 3D technology. Key words to look for with each include:
Light-based imaging modalities: Fluorescence, 3D, technology
Reflectance: Color, red-free, blue, near-infrared
Fluorescence: Autofluorescence, dye angiography
Dr. Dansingani showed the differences in each modality and how something may not be visible on one but evident on another.
Age-Related Macular Degeneration
 Jay Chhablani, MD, Associate Professor of Ophthalmology at the University of Pittsburgh School of Medicine and a vitreo-retina specialist at the University of Pittsburgh Eye Center, discussed age-related macular degeneration (AMD). There are imaging modalities that can be used directly on the tissues. Autofluorescence imaging and multimodal imaging show the progression of AMD.
Jay Chhablani, MD, Associate Professor of Ophthalmology at the University of Pittsburgh School of Medicine and a vitreo-retina specialist at the University of Pittsburgh Eye Center, discussed age-related macular degeneration (AMD). There are imaging modalities that can be used directly on the tissues. Autofluorescence imaging and multimodal imaging show the progression of AMD.
Optical coherence tomography (OCT) angiography shows neovascular membrane progression, which helps physicians decide whether to continue or switch treatment. These modalities are used to quantify changes and as a biomarker.
Dr. Chhablani also talked about artificial intelligence (AI) in retinal imaging. He showed an example of a patient with wet AMD. The 3D technology segments out lesions, quantify them, and then generates a disease profile. The hope is that bringing this information to clinics will allow physicians to follow up on patients more accurately.
Advanced Imaging
 Ethan Rossi, PhD, Assistant Professor of Ophthalmology at the University of Pittsburgh, Assistant Professor of Bioengineering in the Swanson School of Engineering, and Director of the Advanced Ophthalmic Imaging Laboratory, talked about novel techniques being utilized in the advanced retinal imaging lab. He demonstrated the spatial level of detail the imaging can zoom in on (10 times more, and then 10 times more again) to see individual cells of the eye.
Ethan Rossi, PhD, Assistant Professor of Ophthalmology at the University of Pittsburgh, Assistant Professor of Bioengineering in the Swanson School of Engineering, and Director of the Advanced Ophthalmic Imaging Laboratory, talked about novel techniques being utilized in the advanced retinal imaging lab. He demonstrated the spatial level of detail the imaging can zoom in on (10 times more, and then 10 times more again) to see individual cells of the eye.
Adaptive optics improves the contrast with resolution and increased light that makes visible individual cells in the back of the eye. The image moves around because the eye is in constant motion, so a type of image processing is applied to undo this motion. It averages the images to improve the signal, reduce the noise, and get better pictures.
“Another exciting use of this type of technology is for looking at changes over time,” Dr. Rossi said.
One of the things that has made AMD challenging to understand and study is that it is a slowly progressing disease. “Having new, emerging tools that can track the progression is really advantageous,” he added, “because it is helpful not only for us to understand the progression in that particular patient but also helpful as a tool to be able to look at the efficacy of new treatments.”
One new method enhances drusen visibility. Drusen are the defining feature of macular degeneration. Several images are fused to enhance the contrast of the drusen. In comparison with the native image, an increase in contrast of the drusen can be seen.
Dr. Rossi is excited about this new approach, because it is allowing them – they think – to detect some microscopic drusen and structures that are at the earliest stages. These could be the precursors to macular degeneration.
A longitudinal study was done on drusen evolution over a three-year period. The drusen expanded over time and coalesced into one larger shape. The paper on this study was just accepted.
Q&A
One question was if there is any difference in how various imaging modalities are done from a patient perspective. Dr. Rossi said they will all probably feel the same way to the patient. They are relatively quick and different wavelengths of light are used. The major difference would be that research imaging takes a little bit longer than clinical imaging.
When asked how physicians know which imaging to use on each patient, Dr. Dansingani said it comes down to training, understanding, and experience. On the research side, they are always looking to push the boundaries of what they can quantify by applying new combinations of imaging techniques or processing techniques or variations on those.
“One of the things we really want to understand is AMD is progressive at a variable rate,” Dr. Rossi said. “What participants in our studies or what patients in our clinics are the ones who are the greatest risk to developing severe vision loss from AMD. Ideally, we want to catch these at the earliest stages so we can begin to help and prevent progression.”
These new, emerging technologies will also be used to examine conditions other than AMD. Currently there are several ongoing studies using these tools to look at other conditions including inherited retinal degeneration, glaucoma, and other diseases of the outer eye.
With improved detection technologies and less invasive detection technologies, screening will occur at earlier and earlier stages, Dr. Dansingani said. Some of Dr. Rossi’s work is aimed at trying to understand risk factors and how someone’s genotype shapes the structures of the retina. They can potentially begin to build a comprehensive set of biomarkers to see who is at greatest risk for vision loss. “We are not there yet,” Dr. Rossi said, “but we are doing research to set the stage for that.”
Visit https://eyeandear.org/donate to support our research and educational efforts. Please register for the mailing list to stay informed on our research and patient care advances. Should you have any questions please email Craig Smith at craig@eyeandear.org.