Focusing on patient education, patient preferences, and system-based changes to broaden eye care delivery is Dr. Andrew Williams’ passion. The Assistant Professor of Ophthalmology at the University of Pittsburgh talked about “Patient and Community Engagement to Improve Eyecare Delivery in Glaucoma and Other Chronic Eye Diseases” in The Eye & Ear Foundation’s December 17th webinar.
Basic Information About Glaucoma
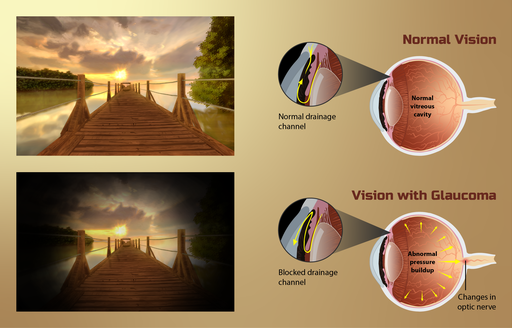
 Dr. Williams started with the basics. What is glaucoma? The technical definition is that it is a disease of the optic nerve characterized by cupping with corresponding visual field loss. People can lose a good amount of vision from glaucoma and have no idea because the brain does such a good job of filling in the gaps. Generally, side vision goes first. This is really dangerous, especially when it comes to driving or crossing the street. There is a risk of falls and other issues.
Dr. Williams started with the basics. What is glaucoma? The technical definition is that it is a disease of the optic nerve characterized by cupping with corresponding visual field loss. People can lose a good amount of vision from glaucoma and have no idea because the brain does such a good job of filling in the gaps. Generally, side vision goes first. This is really dangerous, especially when it comes to driving or crossing the street. There is a risk of falls and other issues.
Glaucoma is a progressive disease in which people are typically asymptomatic until their central vision is lost. This means many people are undiagnosed. And the vision loss is permanent.
Glaucoma is common, affecting two percent of the population over 40. Risk factors include:
- Older age
- Family history
- African American or Latinx heritage
- Intraocular pressure – although 1/3 of patients have normal IOP (<22mmHg)
Treatment includes lowering the intraocular pressure through eye drops, laser, and surgery.
Lack of Patient Community Engagement
Not having patient community engagement is a big problem for glaucoma. After all, as former U.S. Surgeon General C. Everett Koop once said, “Drugs don’t work in patients who don’t take them.”
Dr. Williams described glaucoma as a chronic disease that requires long-term follow-up. A study that looked at loss to follow-up among glaucoma patients over 10 years at a tertiary eye center found that of 428 patients assessed, 395 were included in the study and 132 were lost to follow-up. In other words, 1/3 of glaucoma patients became lost to follow-up over a 10-year period. More severe disease had higher rates of lost to follow-up.
Other risk factors include:
- Travel distance
- Nonwhite race
- Male gender
- Younger age
- Lack of insurance
- Low glaucoma knowledge
The consequences of a lapse in care were severe. Two thirds returned with disease progression or a late surgical complication.
“Loss to follow-up is important and consequential,” Dr. Williams said.
He recently received a grant from the American Academy of Ophthalmology to look at this problem. He will have a database of over a million glaucoma patients.
Follow-up is critical for other chronic eye diseases too. Patients with age-related macular degeneration (AMD) receiving injections with a lapse of more than three months have worse outcomes. One fourth of patients with diabetes have diabetic retinopathy. Early detection and treatment can save their vision, yet less than half receive annual screening eye exams.
How to Help Patients Maintain Care
 Engaging with patients and the community means identifying barriers to care, assessing interventions to address barriers to care, and engaging in outreach. A survey done at a community screening event asked patients about barriers to seeing an eye doctor. “Any barriers” was the response most cited, at 76%. Medical costs were the second highest, at 50%, followed by lack of insurance at 41%. Getting an appointment and difficulties navigating the health system were cited by 10%. Transportation (7%), lack of available services (4%), and language barrier (3%) were other obstacles.
Engaging with patients and the community means identifying barriers to care, assessing interventions to address barriers to care, and engaging in outreach. A survey done at a community screening event asked patients about barriers to seeing an eye doctor. “Any barriers” was the response most cited, at 76%. Medical costs were the second highest, at 50%, followed by lack of insurance at 41%. Getting an appointment and difficulties navigating the health system were cited by 10%. Transportation (7%), lack of available services (4%), and language barrier (3%) were other obstacles.
Barriers to care can be addressed by educating patients. If people don’t realize they have a serious illness, they are unlikely to follow up. “It is really on us to really bring that home,” Dr. Williams said. This means emphasizing the importance of eye care to patients and the community, including conditions like diabetes, glaucoma, and AMD.
“Are we really doing a good job of making sure patients understand what is going on?” Dr. Williams asked.
Connecting patients with available resources is another way to address barriers to care. This is done by providing clear health communication. Dr. Williams wrote a research article on the readability of patient education materials. His suggestions include incorporating the following:
- Active voice
- Limiting dense text; include “white space”
- Clear graphics
A patient navigator is also key. This person is the liaison between the patient, healthcare system, and the community. They connect patients with resources for transportation, financial assistance, insurance, and coordinating appointments. This position is a recent addition to the Department of Ophthalmology.
A similar program at Wills Eye found that 89% of patients desired further contact, 70% found the navigator helpful, and 61% had the issue resolved. Future research will include bringing patient navigator resources to patients at risk of loss to follow-up.
Community Outreach
Community outreach is a third way to address barriers to care. Eye care can be delivered to the community via free clinic sites, primary care offices, and large community screening events. This is one area the Department has been leading for a long time. Dr. Evan Waxman is a huge leader in this area; he developed the Guerrilla Eye Service (now known as Eyes on Wheels) in 2006, which brings comprehensive care exams to primary care clinics at no charge.
A 2019 paper in Clinical Ophthalmology entitled “Delivering mobile eye care to underserved communities while providing training in ophthalmology to medical students: experience of the Guerrilla Eye Service” reviewed 360 patients served by GES. Of that group, 214 were prescribed glasses, 1/3 of diabetic patients had retinopathy. About 1/3 of the patients were referred for further evaluation, with a 72% follow-through rate.
Mission of Mercy is an example of a larger screening event. Held over two days in October 2021, it was a collaboration with dental services. Two hundred and seventy-three patients were seen for eye care, 233 glasses were prescribed and ordered, and 42 follow-up appointments were made.
There is a lot we could do to address in some small way barriers to care. Dr. Williams said. He showed a Venn diagram of social determinants of health or how much it plays a role.
The bottom line:
- Regular follow up is critical for chronic eye diseases
- Numerous barriers to care exist
- Engaging with patients and providing community outreach can scratch the surface of effective public health in eye care
Incremental changes can be made through identifying barriers and addressing them. “I have been passionate about this since I got here in August and am hoping to move the needle just a little bit as I keep going,” Dr. Williams said.
Q & A
The Eye & Ear Foundation CEO Lawton Snyder talked about the EEF mission, which is focused on research. What Dr. Williams discussed is just a different perspective of looking at populations and is also research.
As we invest in resources to help care, that will go a long way, Dr. Williams said.
The Patient Navigator position is recent. Dr. Williams is very interested in data collection to see how effective this position has been. Once enough data has been collected, it will be published and sent to other institutions, departments, and university practices to show that this is something worthwhile and really great for patients. “It is hard to imagine going without at this point,” Dr. Williams said.
One sub-question Dr. Williams is looking at with his grant is how to reach folks best and most effectively, like focusing on the narrower scope of people who are not able to make appointments. He is collaborating with the School of Public Health and is also interested in thinking about broader educational campaigns and their cost effectiveness.
When asked how many cities are tackling these issues, Dr. Williams said there is a real gap. Pittsburgh can become a leader in this area. He hopes to sound the alarm by showing the findings, emphasizing the importance, and then once good clinical data is out, providing a cost analysis and feedback to other institutions. One area he is hoping to explore is getting to where people live, since that is a great way to reach people, provide education, and form relationships to help address barriers.
A good example of innovation is having non eye care providers taking a picture of the back of the eye and sending to an interpreting ophthalmologist. It is not a perfect replacement but is better than nothing.
Visit https://eyeandear.org/donate to support our research and educational efforts. Please register for the mailing list to stay informed on our research and patient care advances. Should you have any questions please email Craig Smith at craig@eyeandear.org.