If you are an organ donor, there is a chance your corneas could be part of a life changing operation.
The Eye & Ear Foundation’s January 28 webinar, “Corneal Transplantation: From Donor to Recipient,” took viewers through the process.
Criteria for Donation
Janice Anderson, Ocular Customer Service Specialist with the Center for Organ Recovery and Education (CORE) Eye Bank, talked about corneal transplants from the donor side. Donors must be between the ages of 2-75 years of age. The following patient conditions do not preclude donor eligibility:
- Cataract surgery
- Glaucoma
- LASIK
- Glasses/contact lenses
- Cancer
There are some exclusions, however:
- Dementia
- Alzheimer’s
- Rabies
- Some behavioral exclusions
Evolution of Cornea Transplants
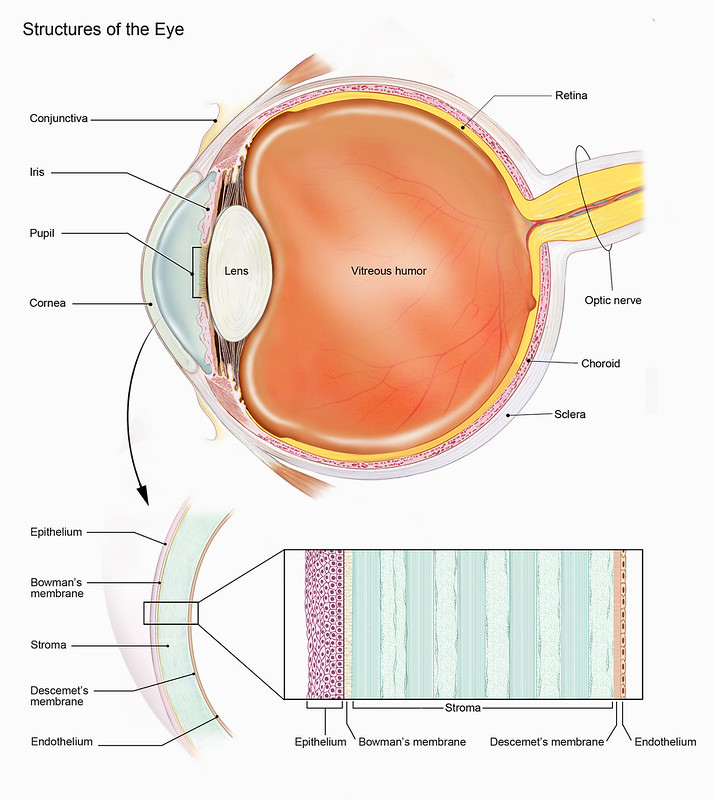
Anderson described the cornea as the outermost part of the eye. It is called the window of the eye and is where light comes through. If it is cloudy or scarred, that affects the rest of the eye. It can impair vision much like trying to look through a glass block window or at a bathroom mirror after a shower.
The first successful cornea transplant was done in Eastern Europe in 1905 by Eduard Zirm, MD. In 1932, R. Townley Patton, MD, established the first eye bank.
Here in Pittsburgh, the Pittsburgh Eye Bank opened in 1952. In 1980, it became the Medical Eye Bank of Western Pennsylvania. In 1996, it evolved into the CORE Eye Bank.
Corneal recovery is an in-situ corneal excision. Generally, only the cornea is removed in a sterile environment. The cross section of the cornea is “really interesting,” Anderson said. It is fairly complex, with several layers. She used the analogy of two business cards on top of each other to demonstrate the approximate thickness of the cornea.
A Slit Lamp is used to view corneas. It can observe defects, abrasions, scars, and other things. What it cannot see too well are endothelial cells, which form a single layer on the bottom of the cornea. A specular microscope is used to see those cells.
For almost 100 years, traditional cornea transplantation meant a full thickness transplant. The surgeon punched out a 7–8-millimeter disc of donor cornea. Now the fancy word for cornea transplant is endothelial keratoplasty. It was discovered that in about 80 percent of patients who needed transplants, endothelial cells were not functioning properly. With this kind of transplant, 90 percent of the cornea is not transplanted. Just 20-25 percent of the “bottom business card” is transplanted – made up of very thin tissue. Only little sutures on the side of the eye are needed, so visual acuity returns quickly.
Preparing a Cornea for Donation
Anderson took viewers through the process of preparing a cornea for donation. The cornea is mounted on an artificial anterior chamber, locked into place with a helmet, pressurized, and then injected into the chamber. Dead cells are removed from the surface of the epithelium, and a measurement of the cornea is taken so they know exactly how much to cut off. Every surgeon has different preferences. The thickness is measured and then marked so it can be put back together.
A turbine with a cutting head and very small blade cuts across the cornea. A mark is made so the surgeon knows top from bottom to position into the eye properly. Another measurement is taken to confirm thickness to the surgeon’s specifications.
The graft is protected and stored in a refrigerator until surgery the next day.
When a full cornea is donated, the cornea is secured and then a guarded punch punches partway through. This allows them to separate the decimal membrane with endothelial cells. The L-shaped instrument works all the way around the cornea, so it is loosened. Then a special forceps is taken to grasp one edge and slowly start pulling it across, about 50 percent. Once it is almost all the way, a small hole is punched. The cornea is flipped over so the epithelium side is up, with the hole opened. That is where the graft goes. An orientation mark of an S is put there for the surgeon, so they know which side is up. The 2-millimeter window created is closed, and the graft goes back into the storage chamber until surgery.
This surgery used to require a lot of sutures and a long recovery time (like several months). Now it is much more stable, and rejection is extremely low because less tissue is involved.
CORE supports local and national research programs to advance the field of medical research. A few of the ocular programs supported include:
- Age related macular degeneration
- Diabetic retinopathy
- Glaucoma
- Stem cell research
CORE also makes available whole eyes and corneas for surgical training and for development of new corneal processing techniques.
Different Kinds of Cornea Transplants
Roheena Kamyar, MD, Clinical Assistant Professor of Ophthalmology at the University of Pittsburgh School of Medicine, discussed corneal transplant surgery from the patient side. Dr. Kamyar is on the advisory board at the Center for Organ Recovery and is the Assistant Medical Director at CORE Eye Bank.
First, she described the cornea as the clear outer layer of the eye, which helps focus light to help you see clearly. It also protects structures inside the eye. Normal thickness is about 540 microns (0.54 millimeters). Layers of the cornea include the epithelium, Bowman’s Layer, Stroma, and Descemet’s Membrane.
Why would someone need a cornea transplant?
- To restore vision in a damaged cornea
- To relieve pain
- Common conditions: swelling of the cornea, inherited conditions (Dystrophies), corneal scars from infections or trauma, thinning of the cornea
There are five types of corneal transplants:
PKP/Penetrating Keratoplasty
- Full thickness corneal transplant procedure
- First one performed in 1905
- Indications: corneal scarring, corneal ectasia (keratoconus or pellucid marginal degeneration), corneal ulceration (infectious or non-infectious)
The good thing about this kind of transplant is that it treats all layers of the cornea. There is a long recovery course, however, with the possibility of rejection. Astigmatism can also occur, requiring the use of rigid gas permeable lenses.
DSAEK/DMEK/Descemet Stripping Automated Endothelial Keratoplasty and Descemet Membrane Endothelial Keratoplasty
In these two types of partial thickness transplants, just the inner lining is removed, which is less than three percent of the entire cornea. DSAEK is thicker than DMEK. This surgery started around 2004.
Indications for this type of transplant include corneal edema due to endothelial disease (Fuchs corneal dystrophy) or psudophakic bullous keratoplasty. Healing time is quick, there is less astigmatism and less risk of rejection, and fewer suture related problems. The major con is that the patient must lay flat after surgery for 1-4 days, depending on the type of surgery and surgeon preferences. This can be very difficult for some patients, Dr. Kamyar said.
DALK/Deep Anterior Lamellar Keratoplasty
This donor graft includes the corneal stoma. It was first performed in the 1970s, but the techniques were refined around 2002. Indications include corneal ectasia (keratoconus, pellucid marginal degeneration), corneal scars that are not full thickness, and corneal stromal dystrophies.
There is less risk of bleeding during this surgery, a stronger wound, and less risk of rejection compared to PKP. But it is a technically challenging surgery and not everyone is a good candidate.
KPRO/Keratoprosthesis KPro
This is a full thickness removal of the cornea and replacement with an artificial cornea. It was approved by the FDA in 1992. Indications include a history of multiple failed grafts, aniridia, chemical injuries, and is considered a “last resort” surgery.
This surgery works very well in many situations where other types of corneal transplants would not work, Dr. Kamyar said. But there can be post-operative complications like infection, glaucoma, or scar tissue behind the optic. As a result, these patients require close follow up. They are seen every 1-2 months. Contact lenses are used to maintain and preserve the prosthesis.
Future Directions for Treatment
Stem cells (note: not embryonic, but the ones in the eye) have promise. The Funderburgh Corneal Regeneration Project has developed a technique with stromal stem cells used in clinical trials for patients with corneal scarring in India. Clinical trials in Japan have shown the benefit of injected endothelial stem cell therapy for Fuchs Corneal Dystrophy and other endothelial cell disorders.
In summary, “There are several different types of corneal transplant surgery,” Dr. Kamyar said. “Your surgeon will help you decide which one is the right one for you.”
Q & A
Cornea transplants should last, on average, about 15 years. Dr. Kamyar has seen them last 30-35 years. It helps if patients take good care of their transplant. It also depends on the disease, as some conditions have a higher rate of rejection.
General anesthesia is used for a full cornea transplant, but usually is not needed for a partial. If a patient wants or needs it, it can be used. A partial transplant is usually short (about an hour to an hour and a half) procedure during which patients stay comfortable. There should not be any pain or discomfort, thanks to the area being numbed.
Patients who undergo a KPro transplant see well within a couple of weeks to a couple of months. A lot of these patients have other conditions that can limit their vision, however, so it depends on how well those are controlled.
CORE has a full department of Donor Family Services, which coordinates communication between donors and recipients. Anderson called it a two-way street. Everyone receives a packet of information and instructions with a card and stamped envelope to encourage them to write a note to the donor family regarding their transplant. A number of patients do this. The cards are sent to CORE, who identifies which donor or family to direct them to. They act as middlemen for a while. Sometimes the donor and recipient actually meet.
As Anderson said at the beginning of her presentation, “Be a hero. Be an organ donor.”