S+S Fall 2022
As an ophthalmologist, Andrew Williams, MD, cares for patients with chronic eye diseases by prescribing medications and performing eye surgery. However, during his training, he realized that much of a disease’s course occurs outside the scope of therapeutics.
For example, he said, a patient with diabetic retinopathy who cannot afford their diabetes medications would return to the clinic with worsened vision due to poorly controlled blood sugar. A patient with glaucoma who loses insurance would be lost to follow up and return later with permanent vision loss.
“The social circumstances in which people live significantly affect their eye health,” Dr. Williams said. “These social factors are broadly described as social determinants of health. Informed by the experiences of my patients, I have driven my research focus into understanding the influence of social determinants of health on vision outcomes. Moreover, the larger goal of my research is to identify mechanisms to address these social factors in order to improve the way we deliver care for patients with social needs.”
A recent collaboration with Department Chair José-Alain Sahel, MD, resulted in an article, “Addressing Social Determinants of Vision Health,” published online in June and in the August 2022 issue of the Ophthalmology and Therapy Journal. Drs. Williams and Sahel set out to examine the existing literature on social determinants of health on vision outcomes.
“This article brings together our perspectives from our unique roles, with my strong research interests in the area and Dr. Sahel’s one-of-a-kind track record in leadership at the intersection of ophthalmology and addressing social needs,” Dr. Williams said. “Dr. Sahel has made access to eye care a priority for the department, and several initiatives have made UPMC Eye Center a national leader in addressing social needs for eye patients. For example, he implemented a patient navigator position in the department, who functions to connect patients with community resources to promote eye health and continued follow up. Additionally, he has worked with community organizations to promote free vision screening through the Mission of Mercy and Vision to Learn initiatives. By putting these programs in the context of published literature, our article provides a unique framework that can promote data-driven expansion of public health initiatives in ophthalmology to address social determinants of health.”
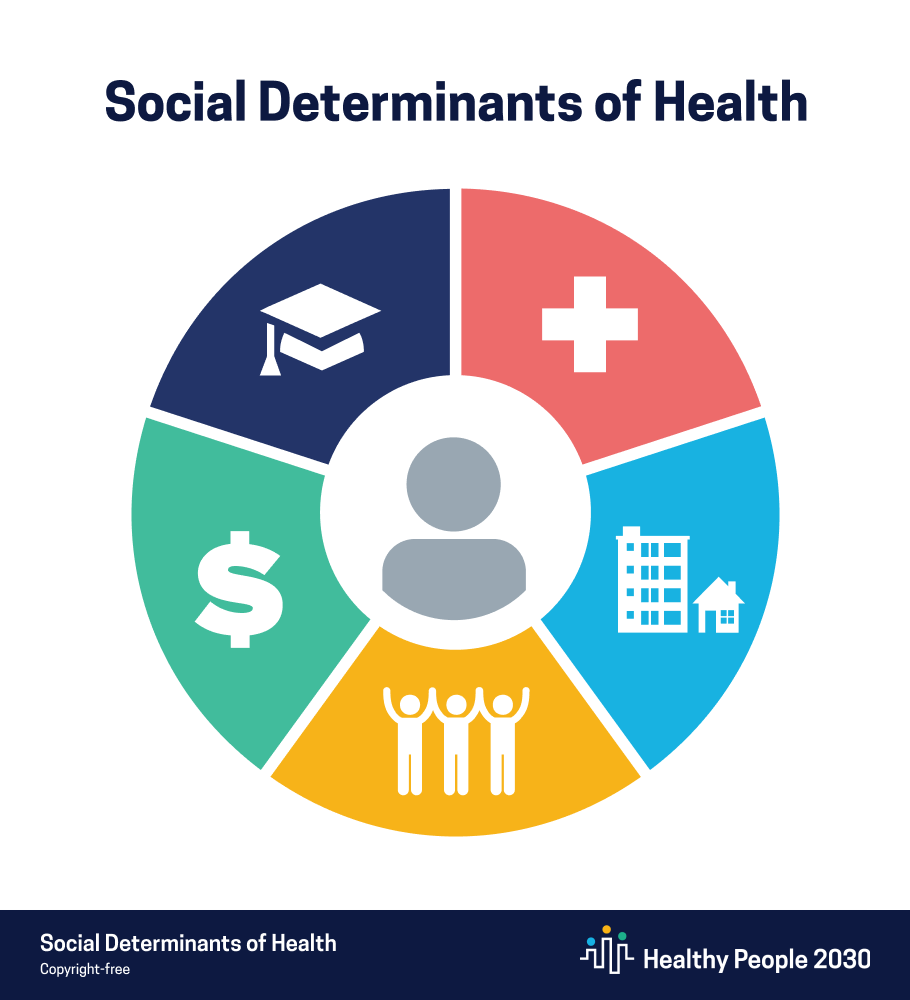
As the article states, “In Healthy People 2030, the U.S. Department of Health and Human Services broadly groups social determinants of health into five domains: economic stability, education access and quality, health care access and quality, neighborhood and built environment, and social and community context.”
Recognizing the gap between understanding the role of social determinants in health and the ability to address these social needs in clinical settings, the National Academies of Sciences, Engineering, and Medicine recently published guidelines to integrate social care with health care delivery. This framework for action has already been adapted by many healthcare providers like dermatologists, internists, and pediatricians. Thanks to Drs. Williams and Sahel, now there is one for ophthalmologists.
The recommendations to address social needs are summarized as the five As: awareness, assistance, adjustment, alignment, and advocacy. “By organizing screening initiatives and community collaborations into a larger framework, we believe that our manuscript can provide an outline for other departments and community practices to bring attention to the critically important social needs of our patients,” Dr. Williams said.
Indeed, Dr. Sahel reported that the paper has had a strong impact. Feedback from other ophthalmologists has been overwhelmingly positive.
“The framework in our article is a constructive starting point for discussion in order to build programs like ours in other settings,” said Dr. Williams.