Dr. Andrew Williams, MD, an Assistant Professor of Ophthalmology who specializes in the medical and surgical treatment of glaucoma and cataracts, called the September 27th Eye & Ear Foundation webinar, “Glaucoma and the Role of a Patient Navigator in Vision Care,” a critically important topic.
What is Glaucoma?
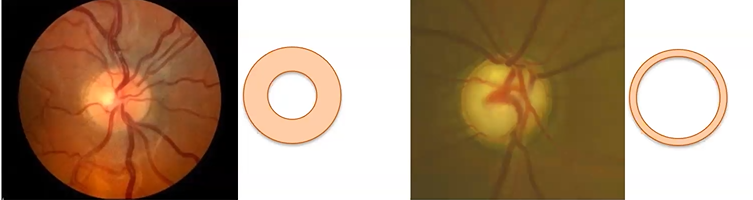
Glaucoma is a disease of the optic nerve characterized by cupping with corresponding visual field loss. The optic nerve is a cable that connects the eye to the brain that erodes over time in patients with glaucoma, leading to loss of peripheral vision. It can eventually result in blindness. As of now, the process cannot be reversed.
Patients notice the loss of their peripheral vision over time, though sometimes it is not noticed until it is already advanced. Their peripheral vision becomes a little fuzzy; the edges are hazy and grayed out. Central vision is maintained until the end.
A tool used to measure field of vision over time is the visual field machine or perimeter. Patients look into a white dome and click a remote when they notice a white light. The machine registers when they notice and when they miss.
Many people are undiagnosed with glaucoma. It typically is not noticed until central vision is lost. Vision loss is permanent.
“Our goal in all treatments is to preserve what’s left,” Dr. Williams said. “This highlights the importance of finding mild cases early and keeping that close follow up over time to prevent patients from getting worse because oftentimes it is left untreated.”
Glaucoma is common, affecting 2% of the population over 40. Risk factors include old age, family history, Black or Hispanic heritage, and intraocular pressure, though 1/3 of patients have normal IOP (<22mmHg).
Glaucoma involves a complex array of genes. If a first-degree relative has it, you have a higher risk. More initiatives are being done in the clinic to address this, asking family members of patients if they have had an exam.
Treatment
Glaucoma is treatable, though not curable. All available treatments work by lowering eye pressure. They involve eye drops (either once or twice a day), laser (done in the office), or surgery (which involves a variety of procedures).
All treatments require monitoring over time, and they can all wear off over time as well. Patients often need more than one treatment.
Lapses in care result in vision loss from undertreatment. Loss to follow up also results in vision loss. Two-thirds of patients who returned after a lapse in care had worsening of their disease.
The important message is that glaucoma is a chronic disease that requires long-term follow up. Unfortunately, loss to follow up is common in glaucoma, occurring in 33% of patients at an academic eye center and 50% of patients in a national ophthalmic registry.
The most vulnerable patients at greatest risk of loss to follow up are the oldest patients, minority racial groups, people with more severe glaucoma, and people with visual impairment and blindness.
Glaucoma and Follow Up
Glaucoma is a chronic, irreversible, and potentially blinding disease that is progressive unless treated. Treatments can preserve vision, but long-term consistent follow up is necessary.
“We need to put a lot of effort into helping our patients care because we often make a diagnosis and situations come up where patients can’t maintain care,” Dr. Williams said. “It’s everyone’s responsibility to give patients the resources they need to help take care of that. It’s a partnership.”
What keeps patients from being able to access care? These are patients who have been diagnosed with glaucoma and are seeing an ophthalmologist yet still have trouble accessing care at regular intervals.
Helping glaucoma patients maintain care means addressing social determinants of health, or specifically, health-related social needs, and understanding reasons for lapses in care. Dr. Williams wrote an article, “Addressing Social Determinants of Vision Health” with Dr. Sahel. Education access and quality, health care access and quality, economic stability, neighborhood and built environment, and social and community context all play a role in access to eye care and risk.
Barriers to Care
Thanks to a grant from the American Glaucoma Society, the Department hired a professional call center to reach patients who missed appointments. They looked at which glaucoma patients had a no-show appointment, which means they had an appointment they did not attend. This is a red flag of becoming lost to follow up.
The call center reached out to 170 patients. About 51 completed the whole questionnaire done via phone. The most common reason they missed an appointment was due to transportation challenges. This included living far away and not driving, lack of transportation, difficulty scheduling a transportation service, or asking the transportation service to pick up on the wrong date. A third expressed interest in talking with a patient navigator.
“We are on the right track to understanding barriers our patients face,” Dr. Williams said.
Patient Navigator
How can the Department help glaucoma patients maintain care? This is where the patient navigator comes in. A liaison between the patient, healthcare system, and the community, the patient navigator connects patients with resources for transportation, financial assistance, insurance, and coordinating appointments.
“Probably more important than any procedure or treatment is to have that patient maintain care,” Dr. Williams said.
Dana McGinnis-Thomas, MHA, joined the team in 2020. Her role is to assist with overcoming any barriers that stand in the way of a patient receiving timely care. She refers patients to resources based on individualized needs. She has lots of referrals in the community. Resources include Area Agency on Aging, Blessed Home Project, Childcare, Changing Lives Through Lenses, Clothing Closet (which she facilitated and manages), Housing, Insurance, Lions Club, Primary Care Physician, Specialty Physicians, TechOWL, Transportation, Utility Assistance Programs, White Cane Program, and YWCA.
McGinnis-Thomas and Drs. Sahel and Williams are co-authors on a 2023 article published in the Journal of Academic Ophthalmology, entitled “Effects of a Patient Navigator Program to Address Barriers to Eye Care at an Academic Ophthalmology Practice.”
In the study done in the first quarter of 2022, a total of 125 patients required assistance with transportation (40%), insurance (26%), and finances (14%). A total of 98% received some form of support, with 90% having their issue resolved. Patients ranked the program highly, with 72% reporting that the program helped with their eye care.
The total number of patients assisted in 2023 was 535. Some referrals include:
- Housing: 5 referrals
- Insurance: 80
- PCPs: 4
- Transportation: 136
- Utility Assistance: 3
Case 1
McGinnis-Thomas shared a case she helped with. A 71-year-old woman had glaucoma but had not had an exam in 10 years. She presented for glasses. Her barriers to care were the recent death of her spouse, poor access to transportation, and she was struggling to maintain her home. She had no working stove or furniture. Her utilities were shut off and she was living in the dark.
McGinnis-Thomas hooked her up with ACCESS and Medical Assistance Transportation Program. She guided her through applications for assistance with People’s Gas/Duquesne Light. She helped acquire household items (stove, furniture, air conditioning), and connected her with rent rebate programs and Meals on Wheels. The Lions Club assisted with new glasses. McGinnis-Thomas also helped her through the death certificate process for her spouse and continued to check in on her after missed appointments.
By addressing the patient’s social needs, she had access to surgery, maintenance of long-term follow up, and stable glaucoma.
Case 2
In another case, a 75-year-old woman had narrow angle glaucoma and could not get to appointments anymore. She had not been driving since her husband developed dementia, and her daughter moved to Germany. McGinnis-Thomas met with the patient and her daughter at their local office, where they discussed ACCESS Transportation, and she helped with the program application. The patient underwent successful cataract surgery and had stable glaucoma upon follow up.
“These are some of the routine kinds of ways that Dana makes a huge impact,” Dr. Williams said. “I’m just one doctor of like 50 here. She does a lot of work for a lot of folks.”
Conclusions
- Glaucoma is a lifelong disease that requires follow up
- Glaucoma patients face barriers to care
- Social determinants of health/health-related social needs
- A patient navigator program can help patients maintain care
- And maintain their sight
“To show such a robust and unique program our Department has through data that [Dana is] leading really illustrates how we can address a lot of these barriers to care and not just give up, but understand patients’ needs and help take care of their eyes for the long-term, ultimately maintaining sight and quality,” Dr. Williams said.
The Department is very unique in that it has a patient navigator who works alongside the ophthalmologists. Dr. Williams is telling ophthalmologists across the country that this is worth doing. “This helps,” he said. “This is a fundamental part of our mission – helping the whole person.”
Photo: Glaucoma is a disease of the optic nerve characterized by cupping with corresponding visual loss. The first image is of a normal eye; the second is one with glaucoma.