A project that the Chair of Ophthalmology at the University of Pittsburgh, Dr. José-Alain Sahel, MD, started in Paris, has continued in Pittsburgh. “We have been fortunate to develop this model of a digital twin that is helping us try to make the right decisions for patients in a very systematic way,” Dr. Sahel said at the start of the Eye & Ear Foundation’s November 18th webinar, “Digital Twin of the Eye.”
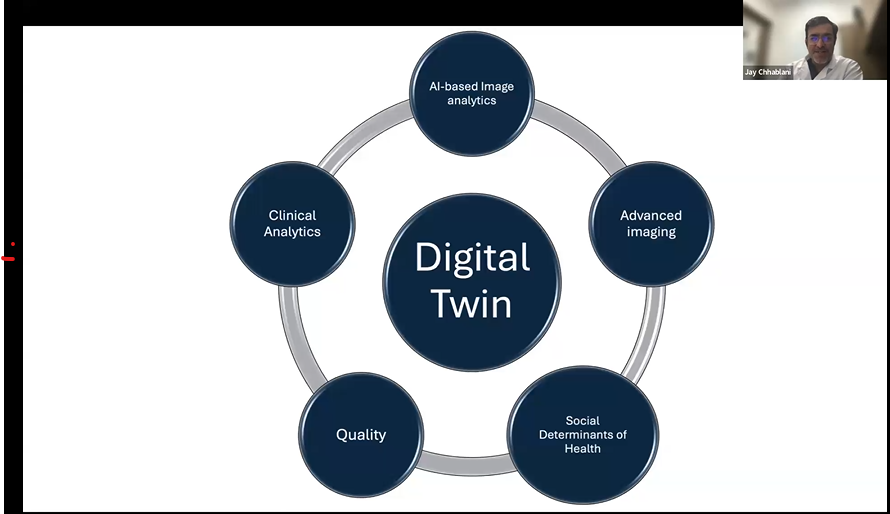
Individualized treatment and safety monitoring are the goals when treating every patient, said Dr. Jay Chhablani, MD, Professor of Ophthalmology and Director of Clinical Research at the Vision Institute. The digital twin model is a complex process in which several factors are used to help offer the best treatment for individual patients. It involves AI-based image analytics, clinical analytics, advanced imaging, quality, and social determinants of health.
Clinical Analytics
The clinical analytics team at UPMC has helped develop an app that allows physicians to see patient details. It addresses which patients are coming to the clinic, how frequently they are coming, and how the emergency visits are. It also logs gender and ethnic distribution and resident zip code, among other things. “It provides us all the possible information, not only about the ophthalmology, but their systemic disease, including all the demographics as well as various factors which can influence the ophthalmologic outcome,” Dr. Chhablani said.
AI-Based Image Analytics
Kiran Vupparaboina, PhD, and Sandeep C. Bollepalli, PhD, work in machine learning and AI. They have created a niche area at the Vision Institute and are working closely on the digital twin, developing interesting technology to treat patients.
AMD
Age-related macular degeneration is a degenerative disease affecting the macula of the retina, an area responsible for high acuity central vision. It is the third leading cause of vision loss worldwide. More than 170 million are affected around the world, and more than 10 million are in the U.S. Both numbers are expected to double by 2050. Risk increases with age, with 2% diagnosed at 50-59 years-old, compared to 30% at 75 years and up. The disease results in $343 billion in global costs; 75% is direct health care.
“This sets up the stage that AMD is something which we are really concerned about,” Dr. Chhablani said. There are two types: dry and wet. Dry means there is no blood but a thinning of the retina. Wet means there is subretinal hemorrhage or some retinal swelling. Monthly or once in two months injections are used for wet AMD. There is lots of research happening in extending treatment and improving treatment outcomes.
Dry AMD is more challenging, however, with no treatment available. However, in the last year, two injections have been approved which can slow down disease progression. For example, if the central area will be affected in 5-7 years, injections can add 2-3 years of good vision. It still is not the best treatment. “We are still trying to improve the outcome,” Dr. Chhablani said. “Is there a way we can prevent before any progression?”
Dr. Chhablani’s lab is focusing primarily on screening as well as predicting the progression of the disease. If it is diagnosed early, vision loss may be prevented, and good vision life extended. His research wants to understand how patients will respond to treatment when converted from dry to wet.
AI-Based Feature Extraction
Instead of being diagnosed by an optometrist and realizing that vision has been lost and there is no hope, the goal is for patients to be screened for AMD. Ideally, there will be algorithms that would identify patients with macular degeneration, and this technology would be used throughout the community for screening.
Blobs in patients with macular degeneration are called Drusen. Identifying these blogs help diagnose the condition before it advances. By using AI techniques, these blobs were segmented. When compared to ground truth image scans, the algorithm had 80% accuracy. “I believe we can improve this further,” Dr. Chhablani said. “Then we will be able to start diagnosing patients in the community. Imagine a day when you can go to Costco and Walmart and get the screening done doing grocery shopping.”
Geographic atrophy (GA) segmentation is seen in a more advanced form of macular degeneration. The algorithm is able to segment the lesion (a patch in the center of vision) and predict how the disease will progress. This wet AMD prediction tool takes information like gender, age, income, marital status, visual acuity, number of comorbidities, and spits out the probability of conversion to wet AMD.
The team is still working on this to further improve the algorithm, aiming to merge the imaging information into this model to make it stronger and able to predict the conversion and progression rates.
Using AI-generated scans to predict is reaching similar accuracy but still being worked on by feeding a lot of data. It will get more accurate with validated software. In the next few years, this should be a reality.
When it comes to dry AMD predictions, images can be synthesized to determine how the patient will look in two years. If compared with real-life data, models are able to predict but need more accuracy. The hope is to achieve this within six months to a year. Physicians will be able to tell their patients the possibility of their vision loss progressing whether or not they undergo treatment.
Advanced Imaging
Ethan Rossi, PhD, leads the Advanced Imaging Lab, where he has multiple tools. Dr. Chhablani works very closely with him. They are trying to image individual cells with high resolution imaging.
Social Determinants of Health
Andrew Williams, MD, a glaucoma specialist, is leading these efforts. Social determinants of health are important because social needs and circumstances affect health and well-being. They predict less access to eye care and poorer visual outcomes. Understanding social factors is key to understanding the course of eye disease.
Initiatives the Department undergoes when it comes to SDoH include screening SDoH at intake. Results are entered into the electronic health record, which facilitates referrals to resources and provides opportunity to incorporate social factors in disease modeling. “SDoH is becoming a crucial component of every treatment modality,” Dr. Chhablani said.
The Department also has a Patient Navigator, whose job it is to help patients who need help with things like insurance, reimbursement, and transport, just to list a few.
Quality
Vishal Jhanji, MD, a corneal specialist is taking care of this quality component. The team wants to understand when patients come to the hospital, what their actual experience is. Do they receive quality care? Are there any complications?
Applications in quality improvement include reviewing operational strategies, capacities, staffing, and care models; identifying areas of improvement and predicting future challenges; optimizing organizational strategies; and reducing “break downs.”
“To offer individualized treatment for our patients, we truly require all these pieces put together to improve the outcome and experience,” Dr. Chhablani said.
Pittsburgh is Unique
The digital twin model is universal. The tools are the same; the system adapts to other conditions. The Department is working on one for retinal degeneration, the cornea, etc. And it is already working on other conditions like diabetic retinopathy and genetic disorders. Because it is a learning system, it improves over time.
While several other ophthalmology departments are working on AI and adapting it to imaging, the Department of Ophthalmology at Pitt is more unique in how it is trying to integrate every parameter. Other centers have contacted Pitt to collaborate. “The goal is really not to work in isolation,” Dr. Sahel said. “We need to share knowledge, because the more data that’s integrated, the more experience you get, and the more patients are involved, the better it’s going to be.”