In the Eye & Ear Foundation’s November 5 webinar, “Tinnitus: Phantom Sounds and Research Updates,” presenters and collaborators Thanos Tzounopoulos, PhD, Director of the Pittsburgh Hearing Research Center and UPMC Endowed Professor of Auditory Physiology, and Gregory Basura, MD, PhD, Director of Global Otolaryngology and Professor in the Department of Otolaryngology-Head & Neck Surgery, talked about their work in trying to understand and find solutions for tinnitus.
Dr. Tzounopoulos explained that tinnitus is a disorder mostly of the auditory system. “I am very fortunate to have created a team here starting 7-8 years ago focusing on different parts of the auditory system,” he said. He called it one of the best teams in the country.
What is Tinnitus?
Tinnitus is a phantom noise often described as “ringing in the ears.” It is usually caused by hearing loss due to loud sound exposure or age. While the condition starts in the ear, it becomes a brain disorder.
Patients typically experience sleep disruption, anxiety, depression, and difficulty with memory and concentration, leading to a significant decrease in quality of life. Up to 80% of patients with severe tinnitus have hyperacusis, an atypical sensitivity to external sounds that leads to the perception of abnormally loud or painful input from the ear.
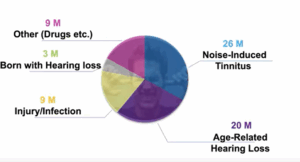
About 50 million Americans have experienced tinnitus.
Understanding Brain Mechanisms
Thanos’ team started studying the dorsal cochlear nucleus, the first stop of the auditory nerve. They found that when peripheral structures are damaged, the brain tries to compensate for lack of input. If the auditory nerve is measured as a function of sound intensity, there is much less hearing response after damage. But different parts of the brain see significant compensation, with the neurons having a strong response.
“If the brain was to compensate for everything, we wouldn’t have hearing loss, but we do,” Dr. Tzounopoulos said. Sometimes when this compensatory process (plasticity) goes astray a bit, it can lead to tinnitus or hyperacusis. Both disorders are associated with brain hyperactivity, likely induced by this plasticity. To understand how it is being developed, the team looked at the auditory brainstem.
Once a neuron is activated, potassium channels are also activated. These channels are major breaks of neuronal activity. In tinnitus, these potassium channels (KCNQ channels) do not function properly, which leads to increased brain activity (hyperactivity).
Drug Development
The team started collaborating with Peter Wipf, PhD, Distinguished Professor of Chemistry at the University of Pittsburgh, to determine whether anything could be done to correct this major mechanism. At the same time as these findings, there was an approved FDA drug that allowed these channels to open. This drug, named retigabine or ezogabine, was used by people with epilepsy. After chronic use, however, it created toxicity. People develop blue skin coloration and blue retina coloration. The drug was removed from the market in 2017.
The next step was to find a molecule that has the same effect on potassium channels but without the negative side effects. In collaboration with Dr. Wipf, the team developed RL-81, which was applied to mice. Even though the drug was applied for a few days, the corrective/mitigating effect on tinnitus and hyperacusis lasted for weeks or months.
The slightly bad news is that RL-81 has some potentially toxic effects, but the team has a new potential lead candidate. However, the money ran out to develop them clinically.
The good news is that a couple of companies have created and developed molecules that have the same mechanism of action on the exact same channels. Drs. Tzounopoulos and Basura have talked to these companies and are getting closer to some deals to have a clinical trial for tinnitus, and perhaps later on for hyperacusis.
Background Noise About Tinnitus
Dr. Basura expanded on the definition of tinnitus, saying it can be subjective or objective. There is an increasing prevalence in the elderly population. Risk factors include exposure to loud noise, lifestyle habits (obesity, smoking, alcohol use, stress), trauma (head injury), arthritis, and drug use (aspirin, antibiotics, quinine, platinum agents).
Mechanisms – Research
Current research includes:
- Brain phenomenon
- Incompletely understood mechanisms
- Abnormal peripheral inputs: cochlea, cochlear nerve
- Dis-inhibition of ascending pathways: DCN/IC/Thal/AC
- Increased central gain: animal models
- Increased spontaneous firing rates
- Increased neural synchrony
- Neural correlates not well translated in humans
The problem is how to study this in humans. There are limitations with current technology. Functional Magnetic Resonance Imaging (fMRI) has a noisy environment. Electroencephalography (EEG) has an electric field that interferes with ERP recording. Emission positron tomography (PET) has radiation that precludes repeated measures.
Theory of Hemodynamic Response
Increased neural activity leads to increased blood floor and increased oxygenated blood and deoxy-/oxy-hemoglobin ratio changes. Thus, an indirect measure of neural activity can be done via hemodynamic response, a “giant pulse oximeter for the brain.” It uses functional-near infrared spectroscopy and is portable, painless, safe, and quiet. However, it can only penetrate to cortical areas. Still, the auditory cortex and other cortical areas are the “end organ” of a lot of processes in the brain and neural response pathways. So, by measuring these and organs, “we can get an index of what is happening on the good and bad side,” Dr. Basura said.
Hypothesis 1
The hypothesis: Tinnitus brains will show increased hemodynamic responses in the auditory cortex. This has been studied since 2016. They have found that the tinnitus brain activates at a much higher level, with much higher oxygen consumption and neurons firing at a higher level all the time. An unexpected discovery was seeing similar activity outside the cortex, in areas not dedicated to direct auditory processing. “This is really exciting and tells us that maybe other parts of the brain that would be seemingly outside the auditory circuit might be contributing to what we are seeing with tinnitus,” Dr. Basura said.
What happens if sound is piped into the system? People who wear hearing aids know that they can sometimes suppress or mask tinnitus. Another novel discovery: hyperactivity is suppressed by broadband noise.
Hypothesis 2
The next hypothesis, in 2017: Tinnitus leads to increased resting state functional connectivity (RSFC) between the auditory cortex and non-auditory regions. The exciting finding showed that compared to a control brain without tinnitus, in someone with tinnitus, multiple areas of the brain – particularly within the temporal lobe where the auditory cortex is housed – has an incredible number of connections going on across the brain, suggesting that the brain is reorganizing itself. This might explain the hemodynamic responses in non-auditory areas.
This data has been replicated, and now the objective changes need to be correlated with subjective reporting. Does the subjective change correlate with an objective change? This is important to map. Dr. Basura is trying to advance capability of measuring different parts of the brain using some adaptive technology. One example is the cap probe, which can replicate responses.
Human Somatic Tinnitus
Experiments are also being done in human somatic tinnitus. Dr. Basura is still conducting these experiments, so it is too early to share data. The somatosensory system of the head and neck feeds into brainstem auditory circuits, and some of these neural correlates can be modulated in animal models by changing the flow of somatosensory or vibrotactile stimulation. In other words, they might be able to modulate perception by moving the head and neck or biting teeth, clenching the jaw, or rubbing the face. Some key pairing orders (auditory and somatosensory) have been identified that suppress neural responses. The fundamental problem is hyperactivity. “If we can find a way – whether it’s potassium channels or changes in flow of circuitry information – to suppress some of this hyperactivity, we may be able to dull or even abate that sound perception,” explained Dr. Basura.
Using somatosensory stimulation in humans with bimodal stems will be exciting to see – looking at the brain in somatosensory variants. Does the brain show similar response patterns? Are different parts of the brain involved? What would that mean for folks that can modulate?
Future Directions
- fNIRS can reliably and repeatedly detect HRs in control and tinnitus auditory cortex and non-auditory cortex; RSFC in tinnitus
- HRs and RSFC may serve as objective “tinnitus correlates” in human tinnitus
- Adapted probes may expand “tinnitus mapping” in humans going forward
- Concurrent animal and human; validate plasticity/identify basic mechanisms
- Somatic tinnitus mapping; create machine algorithms to predict response patterns to design basic science experiments and therapeutic targets
- Tinnitus drug trial
“There are a lot of interesting and really exciting things going on,” concluded Dr. Basura.
